There have been 5,707 studies since 1967 on how well influenza vaccine protects against infection. Many of them did not properly assess whether individuals were infected with influenza, leading to overestimation of the protective effect of vaccines. In many studies a four-fold increase in serum hemagglutinin antibodies were used to confirm infection. Immunization also increases these antibodies, making it difficult to confirm viral infection.
A review of the influenza vaccine studies was done by focusing on reports in which viral infection was confirmed by viral culture or polymerase chain reaction (PCR). The results of 31 studies show that the trivalent inactivated influenza vaccine is overall 59% effective in individuals 18-65 years of age. That means of every 100 individuals immunized, 41 will be susceptible to influenza. This number is far too low – it should be above 90%. The infectious, attenuated vaccine fared better – it is overall 83% effective but only in children 6 months to 7 years of age. It was not significantly effective in protecting individuals 18-49 years old.
Perhaps even more telling is those age groups in which there are no efficacy data for influenza vaccines. No trial results for the inactivated vaccine in 2-17 year olds or adults 65 years and older were considered adequate for inclusion in this study. Furthermore, there were no acceptable data for the attenuated vaccine in the 8-17 year group. Nevertheless, seasonal influenza vaccine is recommended by the Advisory Committee on Immunization practices for all people over 6 months of age.
The 65 and older age group is a main target for influenza immunization to prevent serious illness and mortality. However, there are few data for this age group on the ability of influenza vaccine to reduce illness or death. The infectious attenuated vaccine was shown to have significant efficacy in this age group in only one study, but it is not licensed for use in adults 50 years old or more in the US.
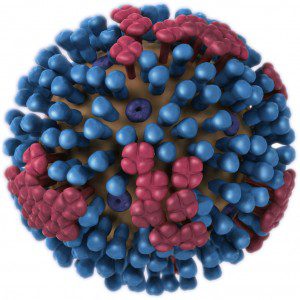
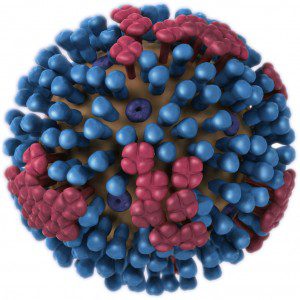
This study sends a strong message that better influenza vaccines must be developed. Why does the inactivated vaccine confer such poor protection? This vaccine is produced by inactivating the virus with formalin and disrupting it with detergents. In this dissociated state it not only does not replicate after intramuscular injection, but it lacks many of the components that induce a strong inflammatory response. Consequently the antibody response is weak. The attenuated influenza vaccine, which replicates in the respiratory tract, is more protective (83%) in the 6 month-7 year age group. If shown to be efficacious in other age groups it would make sense to increase the use of this vaccine, which currently accounts for only 9% of vaccine given in the US. But we should aim for greater than 90% protection and that may require developing entirely new vaccine approaches using novel antigens, delivery systems, and adjuvants.
These findings will provide a rationale for those do not feel it is necessary to be immunized against influenza. But the study authors do not condone abandoning the inactivated influenza vaccine:
€¦We should maintain public support for present vaccines that are the best intervention available for seasonal influenza.
In other words, it’s better than nothing, surely not a ringing endorsement. I suspect that the results of this study will lead to a decline in influenza immunization rates in the US.
Update: Alan Dove has a slightly different view of this study.
Osterholm MT, Kelley NS, Sommer A, & Belongia EA (2011). Efficacy and effectiveness of influenza vaccines: a systematic review and meta-analysis. The Lancet infectious diseases PMID: 22032844

Actually, I heard something about antibody-based “vaccine” in development. It is basically a mixture of two hemagglutinin antibodies, which recognize two different epitope deeper on that molecule, next to membrane, not on the hemagglutinine head. So basically it should work like “broad-spectrum influenza vaccine”.Â
The universal vaccines being investigated would be directed against the conserved HA stalk. Such antibodies have been detected in infected humans and do neutralize a broad range of strains. The epitopes are not efficiently presented in humans and the antibodies are rare; how to elicit them with a vaccine is problematic. See https://virology.ws/2010/10/13/universal-influenza-vaccines/ for more.
Thank you very much. I have found the paper i was reffering to: http://www.sciencemag.org/content/333/6044/843.full . It seems like promising approach to me.Â
Although two anti-HA stem antibodies can neutralize most strains, therapy with antibodies would be far less useful than determining how to immunize to elicit these antibodies in humans.
Pingback: A $607 million investment in cell-based influenza vaccine
But isn’t the 6 month to 7 year old group the largest human reservoir of the seasonal influenza viruses? So won’t an 83% rate be VERY helpful in reducing the incidence in >50 year olds who are more likely to develop serious illness?
Pingback: A $607 million investment in cell-based influenza vaccine | StigmaBot
Pingback: A $707 million investment in cell-based influenza vaccine | StigmaBot
I work at a hospital and am 32 weeks pregnant. If it were my choice, I would not get the influenza vaccine, especially being pregnant. The additives in the vaccine are scary and if they were minimized and only the absolutely necessary ones were in the vaccine, I wouldn’t hesitate as much. For an English homework assignment I have added/posted the following.
Although the influenza vaccine can be beneficial, there are some concerns that come along with it; such as the ingredients, the side effects and who is receiving it. The vaccine has been around for roughly eighty years; through the years more additives have taken their place in the vaccine (NCBI). Influenza vaccines contain numerous ingredients including mercury, MSG, formaldehyde, aluminum, antibiotics and more. These ingredients aid the vaccine’s shelf life and keep them free of unwanted bacteria, as well as potentially harming those who get the vaccine due to the effects they can have on the body. Side effects of the vaccine include runny nose, aches, fever and sore throat. Other, rarer side effects are fainting, pain and limited range of movement where the shot was given, allergic reactions and seizures. Lastly, the vaccine is recommended for those six months and older. While some of ingredients and side effects seem harsh for someone as young as six months or for the elderly, it is still recommended (CDC). Obviously, due to the spontaneity of the influenza virus and the risk of getting the vaccine, one must weigh out the pros and cons when debating on getting the vaccination or not.
“Key Facts About Seasonal Flu Vaccine.†cdc.gov. Centers for Disease Control
and Prevention, 22 October 2014. Web. 19 November 2014.
Pubmed.gov.National Center for Biotechnology Information, U.S. National Library of
Medicine. Web. 19 November 2014.