By David Tuller, DrPH
Update Jan 5, 2023: Martin Rücker, the German investigative journalist who posted the snippets from the draft article, touched base after seeing this post and assured me that the copy he received was not a formally embargoed version provided to reporters before publication. In other words, no embargo was broken, as I had assumed might have been the case. Rücker received the article through a “secure source,” he told me. It is not necessarily clear that the article has already been peer-reviewed or when it might be scheduled for publication.
The usual suspects—several dozen of them—are apparently about to publish a cri de coeur outlining their objections to the ME/CFS guidelines issued in October, 2021, by the UK’s National Institute for Health and Care Excellence (NICE). The upcoming article is expected to appear in the Journal of Neurology, Neurosurgery, and Psychiatry. Not surprisingly, the lead author is our old buddy, Professor Peter White, one of the three main investigators of the now-discredited PACE trial. His PACE co-leads, Professors Michael Sharpe and Trudie Chalder, are also signatories, along with a glittering array of other stars of the biopsychosocial firmament.
Unusually, details about the paper were recently spread around on social media. The source seems to have been an embargoed copy—that is, the advance version of a study often distributed to reporters so they can prepare in-depth reports timed to appear right after journal publication. Of particular note, the authors accuse the NICE committee of having engaged in eight “major errors.”
(In what appears to be a petty show of defiance, the authors insist on using the term CFS/ME, even though the guideline and government agencies in the UK now call the illness ME/CFS. This decision is silly and childish–it makes the authors look out-of-step and clueless.)
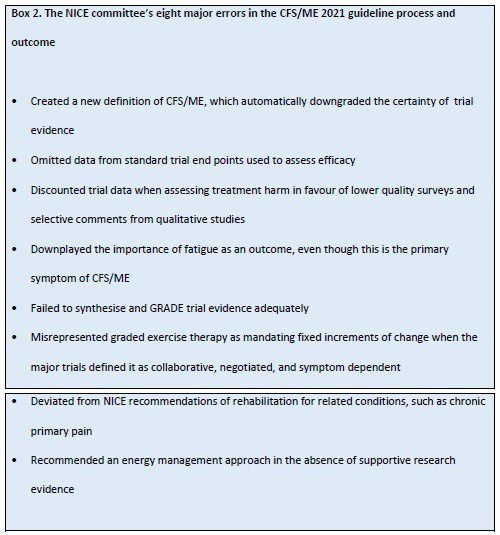
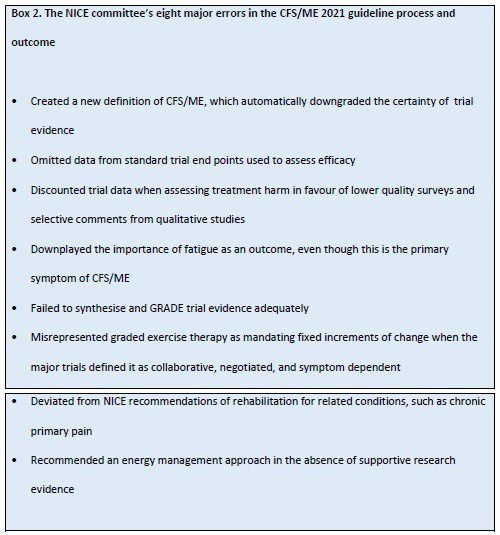
Variations of these tired arguments have already been promoted aggressively by members of the GET/CBT ideological brigades during previous outbursts over the new guidelines. Reprising them again here does not strengthen them. In any event, they have been effectively and repeatedly rebutted.
The authors of the new article seem to believe numbers will bring heft and momentum to their loud collective whine. They are, it would appear, dismayed, perplexed and enraged that the scientific consensus in this field has shifted away from their once-hegemonic views. They know they no longer control the narrative—even as they seek to expand their GET/CBT paradigm to the long Covid domain. It must be a shock to lose relevance in this fashion.
Adam Lowe, a writer in Manchester, England, was one of five patients or patient representatives on the 21-member NICE committee. We spoke earlier today about the eight “major errors” cited by these critics. In our conversation, Adam explained why each item on this list is essentially bogus and unwarranted.

We are very fortunate to have Adam involved in this, knows his stuff and explains it in a clear and relatable way.
I’m not sure how they expect things to go any different than from the roundtable even if anything were to happen. Actually, they should have to explain that, how the roundtable found none of those issues or anything wrong, hence why the publication went through.
I don’t really understand why this piece would be submitted to a neurology journal (if it has been)? The Royal Colleges (or at least the RCPsych and RCGP) previously seemed to regard ME/CFS as a problem for rheumatology, infectious diseases, endocrinology and/or pain clinic specialisms to deal with, rather than neurology – see here -https://www.slideshare.net/jcpmh/guidance-for-commissioners-of-services-for-people-with-medically-unexplained-symptoms (Table 1). Have the Royal Colleges changed their minds on where ME/CFS patients should be referred to, or what? It’s all so confusing. How can doctors possibly keep up?
Thanks Adam and David, for going through those points.
It’s “neurology” as in FND. The journal’s editors include Carson and Stone, who are the biggest proponents of FND (which also, incidentally, uses CBT).
Thank you so much Adam and David. I really appreciate your efforts.
Adam Lowe said:
“It’s “neurology” as in FND. The journal’s editors include Carson and Stone, who are the biggest proponents of FND (which also, incidentally, uses CBT).”
I got that, but this would seem to be a change-about for members of the RCPsych, (if such members are involved), wouldn’t it? Or at least them acting somewhat at odds with how their own college appeared to regard ME/CFS a few years ago? Why would they place ME/CFS with neurology now? I mean, are they now trying to redefine ME/CFS as FND, or something? It looks highly inconsistent to me. Wasn’t IAPT at one time coding ME/CFS patients with ICD-10 F45.0 (which I believe represents ‘somatization disorder’) rather than with the code matching with the WHO’s definition? Has this changed or is it to change? If ME/CFS is now deemed suitable for discussion in a neurology journal, then does this mean that UK ME/CFS patients will all be referred to neurology clinics and coded with a neurology section code? Could they, for example, get coded with “Dissociative Neurological Symptom Disorder” rather than G93.3 or G93.32 or whatever? What is going on here?
what an idiots.
a barrel full of Putins
The trouble with this being published in a journal is that now those around the globe who wish to hold on to the biopsychosocial belief can point to the published piece and simply say, “look, there’s still controversy around this topic. It’s still undecided.”
It says “The upcoming article is expected to appear in the Journal of Neurology, Neurosurgery, and PSYCHIATRY.” I don’t think anything has changed. They are simply digging in their heals as hard as they can to preserve their reputations and their empires.
Thank you David and Adam.
They’re wrong on the primary symptom, as always they’re hung up on fatigue instead of PEM and Exercise/Activity intolerance. This was part of their Oxford criteria, which meant anyone with fatigue could qualify for the PACE Trial whether they had M.E or another fatiguing condition.
Bit rich they say NICE ignore evidence, considering the thousands of papers out there now on M.E & Long Covid which has found evidence and in fact Long Covid research is backing up M.E findings.
On evidence, Psychology has always been about proving a theory. Bio research is about finding actual evidence of biological mechanisms and problems in M.E.
Why do they choose to ignore the undisputable bio research evidence? Oh yeah, it invalidates their ridiculous theories on our fear of exercise.
Let’s hope NICE ignore them.
MELVYN LURIE, M.D.
18 Hobbs Brook Road
Weston, MA 02493
Tel: 617-510-8474, FAX: 617-507-8511, email: mlurie@post.harvard.edu
I am writing to express my appreciation for your articles. They are concise, clear, and cogent. It is important that your perspective be available to the public. I am also writing to ask about your potential interest in receiving one or both of the following: a review copy of–or excerpt from– my book in process, or a related article. The book is about the biology of politics. It allows us to determine where in the civilization cycle we are.
The book explores the genetics behind partisanship as a path toward more productive political discourse. It uses convergent evolution to understand our human species. It’s becoming increasingly difficult to find people who believe we have more in common than we have differences, who believe we can work together for the common good, and who care or are willing to try. Of course, many extremists will not want to move toward political balance. Unfortunately, there will likely be controversy from extremists on both the right and the left.
I have experience in politics on a national level, including serving as a field director for a U.S. presidential election. However, what I believe has most enabled me to understand politics is my experience in genetics, which began with studies at Johns Hopkins University, followed by Harvard Medical School, where I won Harvard’s Reznick Prize for Research for my work at the Pasteur Institute in Paris.
I’ve also benefitted from my time as a practicing psychiatrist, which has helped me understand and appreciate even greater depths regarding human nature and what all of us have in common. What I’ve discovered is different than what others knowledgeable about psychology and political theory say–as well as the media.
My frustration with the seemingly endless onslaught of political confrontations and conflict throughout our country spurred me to discover that the best government is one most aligned with human nature. Not how we define human nature, but how nature defines it. To do so, I draw new political parallels between our human species and certain animal species.
My first book was published by Random House/Dorling Kindersley (DK), and I have not yet started contacting publishers who might be interested in this one. However, I wanted to connect with you while I’m still working on it to ask about your interest in receiving a review copy, excerpt, and/or related article either now or in the future.
I believe you and your audience would be interested, and, as you might imagine, I would greatly appreciate any kind or constructive comments.
With appreciation,
Melvyn Lurie, M.D.
Board Certified by The American Board of Psychiatry and Neurology
https://www.positivehealth.com/article/cfs-me-long-covid/medically-unexplained-symptoms-diverting-5-year-funding-from-mental-health
This article goes into the ways that this lot are now putting ME/CFS under a large umbrella along with a range of other conditions under the spurious idea that if a condition is not ‘medically explained’, it magically becomes a psychiatric condition. You do this simply by adding initial capitals! Medically Unexplained Symptoms: MUS.
In fact, these conditions, occurring in people with no narrative that would provide an explanation for developing a mental health problem (happy childhood, socially, academically and athletically successful – look at the CV of almost any child or adult who has become severely ill, such as in Voices From The Shadows), are clearly Psychiatrically Unexplained!
The use of ME’CFS v CFS/ME is part of the effort on the part of these people to keep the focus on ‘fatigue’ (which occurs in many illnesses) and to delete ME as a separate diagnostic entity. In an undated letter from Strauss to Fukuda (from the time when the CDC was dismissing the Lake Tahoe epidemic), Strauss congratulates Fukuda on having created a set of diagnostic criteria, focusing on fatigue, thus making it possible to lose the concept of ME as a separate condition, an outcome which he regarded as desirable.
Simon Wessely has written something similar about using the term CFS/ME, also with the intention and hope of losing the ‘ME’ bit and keeping the focus on fatigue.
I’ve been following research for thirty years now, including referring to the CDC information on ME and CFS, which has changed over the years. The two things were linked for a long time. Then there was a period when their information was only about ‘CFS’, with a footnote saying that this illness was sometimes called ME, Myalgic Encephalomyelitis. But when you looked for Myalgic Encephalomyelitis, it simply took you back to the CFS page.
A few years later, there was no reference at all to Myalgic Encephalomyelitis. As the CDC is the source of diagnostic categories for US doctors, this meant that every patient who had ME in the US would be given the diagnosis CFS. I came across patients in the US who had never heard of ME, thus had no access to information about ME. It is for this reason that I continue to use ME/CFS rather than just ME when writing about this illness.
On whether GET causes harms, in the old guidelines (CG53), in the section about GET as treatment, there is a bit about managing ‘setbacks’. It refers to pausing GET during a ‘setback’, until the patient gets back to his previous baseline, if they do. This is an admission that after a ‘setback’ during treatment, there will be some patients who do not get back to their previous level of function. They clearly know that during treatment some patients will be made irreversibly worse.
I think we need to ditch the term ‘fatigue’. It is muscle failure after minimal exertion. And Post Exertional Malaise isn’t ‘malaise’ (unease). It is worsening of all symptoms.
So glad the IOM criteria are being used – in the last sentence before the recommendation for the name ‘systemic exertion intolerance disease’, is states that the name is meant to signify that the defining feature of this illness is that ‘exertion may adversely affect many body systems’ – Which I take to mean ‘may damage’, and the recognition that it isn’t just any specific organ, but ‘many’, not just one, and ‘systems’, not just organs.
And it’s disturbing that the NHS are offering Long Covid treatment programs based in local gyms, which provide ‘psychological support’, and rehabilitation exercises, urging patients to ‘push through’ – what does this sound like to you?
I hope the neuropsych brigade pull apart all the flaws or holes in this guideline for misdiagnosed fatigued patients. Even these buffoons should have no trouble in doing that. The guideline is not supportable and its indefensible. Idiots are the only ones supporting a guideline that will lead to disability or even deaths. I reckon this guideline will end up getting pulled at some point. Its a bad guideline written by people who dont know what they are talking about. Too many problems with it. Its based on a vague definition that represents an imaginary disease for a start. The patients are misdiagnosed. Certainly not a Myalgic Encephalomyelitis guideline. So I have no idea why the term is even attached. These aint M.E. Patients. Misdiagnosed CFS patients. Its a heterogeneous group of mostly uninvestigated patients. This is not directed at a single patient with Epidemic M.E. yet the term is attached. The patient group this is directed at. None of them have M.E.. Genuine ME patients are excluded from the guideline; under consider another diagnosis. Joke Guideline. As harmful as the last. Worse. As not even learnt by past mistakes but repeated the same errors again. Its blatant fraud. Written by fraudsters and con artists. Bad people wrote this guideline. Simple as that.
Epidemic ME and Chronic Fatigue Syndromes aint even the same patient groups Nancy. CFS is a misdiagnosis. The guideline has nothing to do with bonafide ME patients. As Greg who left the guideline early couldnt condone this guideline as his wife has ME and who is not in the misdiagnosed fatigued group of patients; that this guideline is directed at or aimed at. The guideline is harmful so its of no wonder why he left. Not supportable by sane people. Its possible many of these patients have had acute limbic injuries, myopathies & neuropathies or even a chronic infection involved leading to disability. It wont help this group of patients to receive prompt medical care upon falling unwell. Acute injuries need to be treated upon onset or an infection which persists. Its a disaster of a guideline. Certainly not a guideline directed towards M.E.. They dont know whats wrong with these patients. Causes unknown. All they know is they presented with Fatigue. Nothing to do with M.E.. Uninvestigated and Misdiagnosed as ME/CFS doesnt exist as a medical diagnosis with diagnostic tests that can be repeated. Its a scam.