by Gertrud U. Rey
Have you ever wondered what would happen if you were infected with two different viruses at the same time? A recent study aimed at addressing this question has produced some astounding new findings.
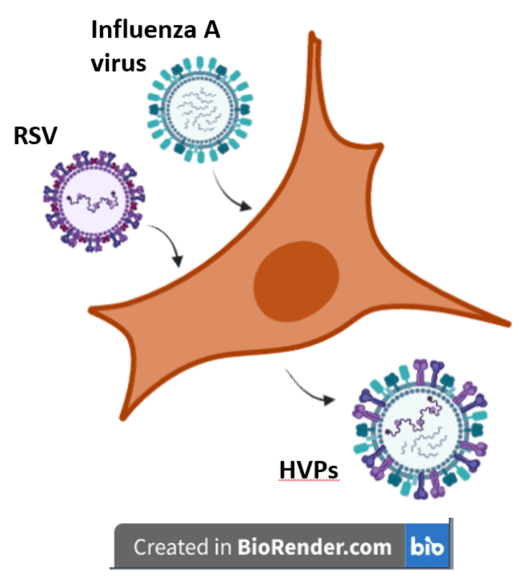
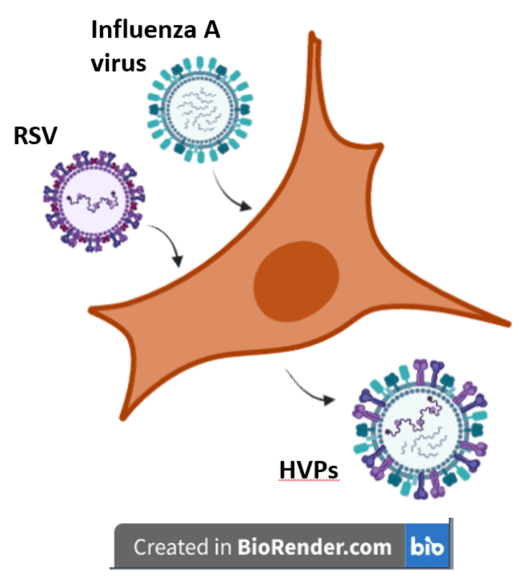
The authors of the study wanted to observe the interactions between respiratory syncytial virus (RSV) and influenza A virus (IAV), so they infected lung cells with either virus or a mixture of both viruses. An initial experiment comparing the replication kinetics of each virus in co-infected cells to those infected with either virus showed that co-infection had no impact on the replication of IAV, but did lead to reduced replication of RSV.
IAV and RSV each localize to distinct cellular regions during their individual courses of infection – RSV aggregates in cytoplasmic complexes known as inclusion bodies, and IAV scatters more diffusely throughout the cytoplasm. Analysis of infected cells by fluorescence microscopy using antibodies against both the RSV and IAV nucleoproteins revealed that co-infection did not alter this localization – RSV was still in inclusion bodies and IAV was diffuse. The authors then analyzed later stages of infection, when in single infections, these viruses assemble in structures called lipid rafts in the plasma membrane. Their results using antibodies against the IAV hemagglutinin (HA) protein or the RSV F protein (i.e., the viral surface glycoproteins) revealed that in co-infections, both viruses were also simultaneously in the same region around the plasma membrane, suggesting that viral particles budding from the cell surface could contain components of both RSV and IAV.
Using high resolution confocal microscopy and a technique known as cryo-electron tomography, which reconstructs a series of image slices to generate a three-dimensional structure of a sample, the authors found that co-infection of cells produced two types of particles. The first type, called ‘pseudotyped viruses,’ consisted of RSV particles with IAV glycoproteins. The second type, designated ‘hybrid virus particles’ (HVPs), were true hybrids containing the genomes and surface glycoproteins of both viruses with distinct structural regions characteristic of each virus. Because glycoproteins determine which cells and cell surface proteins viruses can bind to (i.e., their “antigenicity”), it is reasonable to assume that HVPs would have a modified antigenicity relative to IAV and RSV. IAV entry into cells occurs via the viral HA protein, which binds the cell surface protein sialic acid. RSV entry is effected in part via its F protein, which mediates fusion of the virus with the host cell membrane. To determine whether the HA and F glycoproteins on the HVPs were altered in terms of their antigenicity, the authors carried out a neutralization assay, which reveals whether an antibody can bind a glycoprotein and inactivate the viral particle. Anti-HA antibodies neutralized HVPs about three-fold less efficiently than viruses collected from cells that had only been infected with IAV, suggesting that the HA on HVPs is different enough so that antibodies won’t recognize it. In contrast, anti-F antibodies neutralized HVPs about as well as they did viruses isolated from cells infected with RSV only, suggesting that the antigenicity of the F glycoprotein on HVPs was well preserved. These results also suggested that HVPs cannot enter host cells using the IAV HA protein, and likely enters via the RSV F protein instead.
To test this hypothesis, the authors treated cells with neuraminidase, which binds sialic acid and sequesters it, thus leaving no receptor for IAV to bind to and enter the cell. Viruses isolated from singly or co-infected cells were then used to infect these neuraminidase-treated cells, and the cells were stained with IAV and RSV nucleoprotein-specific fluorescent antibodies and visualized by fluorescence microscopy to determine whether IAV, RSV, or HVPs had infected them. As expected, neuraminidase-treated cells infected with viruses isolated from RSV only- or IAV only-infected cells contained RSV nucleoprotein but not IAV nucleoprotein, suggesting that IAV was unable to infect these cells (because there was no sialic acid to bind to), while RSV infected these cells normally because RSV entry is not dependent on sialic acid. Interestingly, neuraminidase-treated cells infected with viruses isolated from co-infected cells contained an abundance of IAV nucleoproteins, further implying that HVPs containing IAV genomes entered these cells using RSV F protein.
To confirm that the RSV F protein mediated HVP entry into cells, viruses isolated from co-infected cells were treated with a monoclonal antibody against RSV F protein before they were used to infect neuraminidase-treated cells. The monoclonal antibody would presumably sequester any viruses having the F protein and prevent any F protein-mediated entry into cells. This treatment led to significantly reduced entry of HVPs into cells, confirming that the RSV F protein mediates entry of hybrid particles into cells.
Studies of virus-host interactions are extremely common, and scientists have made a lot of progress in understanding the mechanisms that drive these interactions. In stark contrast, we know very little about how viruses interact with each other. Some work has shown that not all co-infections are successful and often result in “competitive exclusion,” with one virus displacing the other, thereby preventing it from completing a replication cycle or establishing an infection in the first place. To my knowledge, this is the first study showing that two completely different viruses can coordinate their replication cycles to develop some kind of symbiosis in a clear display of co-evolution. And although this phenomenon may seem extraordinary, it is probably more common than we think.
[For a more detailed discussion of this study, please check out TWiV 958. The material in this blog post is also covered in Catch This Episode 43.]

Purnell Choppin’s lab first showed pseudo type formation between different RNA viruses. Our lab confirmed these results and extended them to retroviruses and between DNA and RNA enveloped viruses.
@Alice – could you please provide a link to published work, if available? That sounds very interesting!
Gertrude:
Here they are. Hope they are helpful..
Huang, AS, Besmer, P, Chu, L and Baltimore, D: Growth of pseudotypes of vesicular stomatitis virus with N-tropic murine leukemia virus coats in cells resistant to N-tropic viruses. J. Virol. 12:659-662, 1973. PMID: 4355863
Zhu, Z, Chen, SSL, and Huang, AS: Phenotypic Mixing between human immunodeficiency virus and vesicular stomatitis virus or herpes simplex virus. J. Acquired Immunodeficiency Syndromes, 3:215-219, 1990. PMID: 2154577
Very innovative thoughts. We have a large catalog supporting virus research. And currently, there is a promotion event https://www.bocsci.com/get-500-vouchers.html. Hope the efforts we make can advance virus study projects.
Opposites attract? opposites attack?
Ok, ok … just different … but do they go into the same cell to become born again,
or do they go their separate ways?
RE: my comment above.
Vince, the one who knows most about this issue, indicates that viruses at phase one are not, repeat, are not alive.
However, Vince goes on further to say that they are alive in phase two.
Thus, this “When Two Different Viruses Have Offspring” discussion has me wondering if they do this in phase one or phase two?
And possibly more importantly, do they do it as a couple or as singles (Are Viruses Alive)?