by Gertrud U. Rey
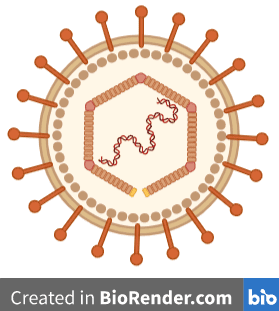
Epstein-Barr virus (EBV) is a prevalent human herpesvirus that is most commonly transmitted through saliva and is well known for causing infectious mononucleosis (i.e., “mono”). Various recent lines of evidence suggest that EBV infection may also be a risk factor for the development of multiple sclerosis (MS), an autoimmune disease in which the protective covering of nerves is progressively damaged, leading to severe neurological problems.
In an effort to identify a possible causal link between EBV infection and MS, several research groups collaborated with the US military in an impressive epidemiological survey spanning a 20-year period. The study drew from a population of more than 10 million military personnel. The authors then investigated/documented 801 subjects who had developed MS during the course of service. Active duty members are routinely screened for HIV infection at the start of service and every two years thereafter, and residual serum samples are stored in an archive at the Department of Defense. The authors analyzed up to three of these residual samples from each person who had developed MS after entering service for the presence of antibodies against EBV. As a control, they also screened the samples for antibodies against cytomegalovirus, another common human herpesvirus that is also transmitted through saliva but that has no known causal link to MS. Remarkably, only one of the 801 MS subjects was EBV-negative at the time of the last sample – all others had tested positive for EBV at some time prior to onset of MS but had been EBV negative when they first joined the service. The presence of EBV antibodies in the serum by the time the third sample was drawn was associated with a 32-fold increased risk of developing MS, with a median time interval of 7.5 years from estimated EBV infection to onset of MS, suggesting that EBV infection was a causal factor for the development of MS. In contrast, there was no correlation between cytomegalovirus infection and development of MS. In fact, the risk of developing MS was lower for people who had been previously infected with cytomegalovirus.
Based in part on these results, the authors of a different study aimed to identify a molecular mechanism by which EBV ultimately leads to the development of MS. Because MS patients almost always have high levels of antibodies against the EBV protein Epstein-Barr nuclear antigen 1 (EBNA1), it is possible that these antibodies cross-react to self antigens with similar amino acid sequences in an autoimmune mechanism known as “molecular mimicry.” One such self antigen with sequence similarity to EBNA1 is GlialCAM, a protein produced by cells of the central nervous system, where it mediates the binding of cells to each other and their surrounding materials.
As a first step, the authors collected serum and cerebrospinal fluid (CSF) samples from MS patients and control patients suffering from a non-MS neuroinflammatory condition. They then isolated single B cells from each of these samples and analyzed the cells for the presence of membrane-bound antibodies (i.e., B cell receptors) that are characteristic of MS. B cells isolated from the CSF of MS patients displayed a range of B cell receptors that were not present in the sera of these patients or the CSF or sera of non-MS patients, a disparity that is indicative of central nervous system inflammation and a hallmark of MS. When the genes encoding these B cell receptors were sequenced, they were found to be highly clonal, meaning that there were only a few different sequences present, with each sequence present in large numbers of copies or “clones.” In other words, the clonal antibodies were the offspring of only a few select precursor B cells that were repeatedly expanded within the CSF of MS patients. In contrast, the sequences of B cell receptor genes from the CSF of non-MS patients were mostly different from each other (i.e., non-clonal). This finding suggested that the antibody-encoding gene sequences in the B cells of MS patients were undergoing a process called somatic hypermutation – a rearrangement of the original germline sequences that leads to an optimized antibody response. And although somatic hypermutation typically occurs in the germinal centers of lymphoid tissues, in MS patients it seemed to be happening in the CSF.
Antibodies that were secreted from B cells in the CSF of MS patients were isolated and characterized by mass spectrometry, a technique that reveals the chemical identity of molecules and the amino acid composition of protein peptides. The amino acid sequences of these antibodies were then compared/matched to the previously sequenced B cell receptor genes to determine whether these antibodies originated from those B cell receptors. This comparison revealed that for 87% of the clonal B cell receptor sequences, the CSF of MS patients contained matching peptide sequences that were unique to the patient. In contrast, only 40% of the non-clonal sequences had matching peptides in the CSF. Antibodies that were highly abundant in the CSF matched to a few clonally expanded B cell receptors, confirming that a small fraction of B cells produced most of the antibodies in the CSF.
As a next step, the authors generated monoclonal antibodies from each of 148 individual B cell receptors isolated from the CSF of MS patients and tested their ability to bind EBNA1. Antibodies from six out of nine MS patients bound full EBNA1 protein, and antibodies from eight of those nine patients bound shorter peptides of EBNA1. One of these monoclonal antibodies, called MS39p2w174 (shortened here to “MS39”), bound EBNA1 in a region that was previously shown to induce stronger antibody responses in subjects with MS than in healthy individuals, and was thus used in all subsequent binding studies. Comparison of the amino acid sequence of MS39 to that of the known wild type version of this antibody (i.e., “germline MS39”) revealed that only two of the amino acids in MS39 that interact with EBNA1 were different from those found in germline MS39, suggesting that only these two amino acids resulted from gene rearrangement during somatic hypermutation. Because the remaining sequence of this “hypermutated MS39” was identical to the sequence of germline MS39, it is likely that naïve B cells producing germline MS39 can bind EBNA1.
MS39 also bound GlialCAM, although this binding was significantly reduced for germline MS39 compared to hypermutated MS39. In contrast, both germline and hypermutated MS39 bound EBNA1 with similar affinity. This observation suggested that somatic hypermutation of MS39 increased its binding affinity for GlialCAM.
A comparison of hypermutated MS39 binding affinity to whole EBNA1 protein, whole GlialCAM protein, and shorter peptide versions of EBNA1 and GlialCAM revealed that the antibody bound both versions of EBNA1 with equal affinity but bound whole GlialCAM much more strongly than its peptide version. In its native state, GlialCAM protein is heavily phosphorylated – a modification that is mediated by a group of enzymes called kinases, which attach phosphoryl groups to certain amino acids. When the authors phosphorylated two specific amino acids on GlialCAM, the binding affinity of hypermutated MS39 to GlialCAM increased by at least 50-fold. Considering that certain kinases are known risk factors for MS, it makes sense that phosphorylation of GlialCAM by these kinases would lead to an increased ability of hypermutated MS39 to cross-react with GlialCAM, thereby potentially leading to MS.
The authors also tested plasma samples from MS patients and healthy individuals for their reactivity to EBNA1 and GlialCAM. Plasma from all MS patients and most healthy individuals were reactive to EBNA1, suggesting that all of these samples contained antibodies to EBNA1 protein. However, only plasma from MS patients had any significant reactivity to GlialCAM, suggesting that only MS patients have antibodies that bind GlialCAM with high affinity. This confirms that there is likely a molecular mechanism that causes MS patients to develop antibodies that target and attack GlialCAM.
Considering that EBV infects about 95% of adults, it is currently unclear why most people never develop MS. However, because humans all have different cell surface molecules that present antigens to cells of the immune system, it is possible that different people present different portions of EBNA1 and/or GlialCAM on their cell surfaces, resulting in varied B and T cell responses that lead to different immune outcomes. Despite the low incidence of MS, it would be great to have a vaccine that prevents EBV infection, thereby possibly also preventing MS.
[For a more detailed discussion of these two papers, please check out TWiV 869.]

Pingback: A Viral Risk Factor for Multiple Sclerosis | News I Can
It’s TIME for a vaccine against Epstein -Barr!!!! I have been advocating for this for over a decade.
Epstein is an Oncovirus and it is unconscionable that we do not have one.
I SEEMS IT IS TRUE – WHY BEAT WHEN YOU CAN TREAT $$$$$$