The emergence and spread throughout Europe of a SARS-CoV-2 variant, 20E (EU1) in the summer of 2020 illustrates how a virus may become dominant not by increased transmissibility but through travel and lack of effective containment and screening.
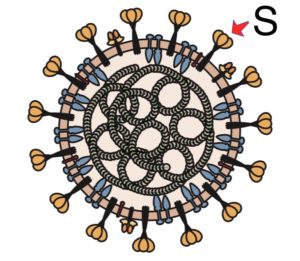
The SARS-CoV-2 variant 20E (EU1) emerged in Spain in the summer of 2020 and spread to multiple European countries. By the fall of 2020 most of the sequences in Europe were from 20E (EU1). The variant bears a number of amino acid changes including A222V in the N-terminal domain of the spike protein (pictured).
Results of binding and neutralization assays revealed that the A222V change did not affect interaction of the spike protein with polyclonal or monoclonal antibodies. Lentivirus particles bearing the spike with A222V did not reproduce with higher efficiency in cells in culture. Authors conclude that these observations are not consistent with increased transmissibility of the 20E (EU1) variant. However, I would argue that studying the infectivity of a pseudotyped virus – in this case a lentivirus bearing the SARS-CoV-2 spike – in 293 cells (possibly human embryonic kidney) has virtually no relevance to what occurs in humans. At the very least, authentic SARS-CoV-2 infection of human respiratory tract cells must be examined. Even then, the results may have no direct bearing on what occurs in humans.
In contrast, epidemiological evidence explains the spread of 20E (EU1). This variant arose first in Spain in early summer 2020. It then spread extensively in Spain and also spread to other European countries. Results of modeling indicate that the spread of the variant can be explained by holiday travel-associated transmission (many EU countries opened their borders to travel on 15 June), and human behaviors such as failure to distance, mask, restrict gatherings, and adequately test for infections.
It seems likely that human behavior might also account for the global spread of other SARS-CoV-2 variants (e.g. alpha and beta). Authors believe that such spread is due to increased inherent transmission of the viruses, but the data in support of this conclusion are not convincing. Increased reproduction of pseudotyped viruses in cells in culture, as pointed out above, is likely irrelevant. Increased shedding of viral RNA from the nasopharynx, detected by PCR, is also irrelevant as it does not represent infectious virus. In no case has shedding of infectious virus from the nasopharyngeal tract been studied to address potential mechanisms of increased transmission. It is claimed that the reproductive index of variants is increased, but these calculations are flawed. The reproductive index is determined by a formula that includes both viral and host factors. However, host factors are never included when this index is determined for individual variants. As the study above indicates, human activities can substantially affect predominance of a virus in a population.
Why do variants out-compete and displace other viruses? It is because the variants have increased fitness, the ability of a virus to reproduce in the host. Fitness can be altered in many ways, including evasion of antibody responses, increased particle stability, and even person to person transmission. No experiments have been done to explain the increased fitness of variants. Fitness is not the same as transmission.
Variants of influenza virus arise frequently, and these variants displace existing viruses because they have a fitness advantage. For influenza virus, a fitness advantage is often conferred by HA amino acid changes that allow escape from antibody neutralization. Antigenic variants can infect a slightly larger number of hosts and that is enough natural selection advantage for the new variants to outcompete the older ones. No one ever says that these influenza virus variants have increased transmission.
Unfortunately the narrative that the variants have increased transmission is dominating the media. This situation has arisen because virologists, epidemiologists, and evolutionary biologists are not talking to one another. In addition, what we know about other viruses, as illustrated here for influenza virus, is also ignored.

Pingback: Holiday travel explains spread of a SARS-CoV-2 variant - Virology Hub
Dear Prof Vincent, You are probably right again. But the point is, just saying that people can’t crowd together or it will facilitate the viral spread is like telling the story of Little Red Riding Hood without the big bad wolf. In this case, the big bad wolf is the increase in transmissibility of the new variants. I think this is important as it makes it easier to influence public policies on lockdown and international travel bans. However, the summer holidays undoubtedly influenced the spread of the gamma variant in Brazil.
I feel there’s a bit of a gap in the reasoning of the original post.
There are seem to be two separate things whose cause is in dispute:
A) the change over time in the total number of SARS-CoV-2 cases
B) the change over time in the proportion of cases due to particular variants.
Now, I take the point that the change in the total number of cases might be down to any number of factors besides biological differences between virus variants, such as people going on their summer holidays proving increased opportunity for the virus to spread.
The change in the proportion of cases due to particular variants is a different matter. Is the argument in the original post that this is just due to founder effect, rather than natural selection? E.g. the people going on their summer holidays travelled to regions where particular variants just happened to be prevalent by chance, even though those variants had no selective advantage?
The statistics of this is kind of interesting … if the null hypothesis is that variants are selectively neutral, but we have clusters of cases due to one person going on holiday, becoming infected with a random choice of variant, and coming back to infect lots of others, who in turn infect lots of others… what statistical distribution of variants do we expect?
The newspapers are reporting that there is likely to be a UK government announcement delaying the easing of UK lockdown.
The variants are possibly serving as a kind of excuse for the politicians to change plan.
“Cases are going up faster than we planned for, so we’re delaying the easing of lockdown” seems reasonable to me, and doesn’t say anything that looks obviously false.
“Cases are going up faster than we planned for *due to the new variants*, so we’re delaying the easing of lockdown” contains a claim about causes that – see Prof. Rancaniello’s recent post – might not be true.
If the stated reason for the policy change — cases are going up — is true, then (from a government planning point of view) it possibly doesn’t matter all that much which out of several possible causes has made the number of cases rise.
But yes, I can see the scientists have reason to complain if the politicians are justifying policy changes with alleged scientific findings that might not be true.
In addition, Vincent, R0 is widely abused in scientific discussion about infectious disease. It is a mathematical fiction that does not exist in the real world. Understanding this makes the concept of how variants can climb a scale-free network to become dominant much easier to understand. This blog post has a diagram that shows a real scale-free network. All of that activity is compressed by R0 into one number.
https://brianhanley.medium.com/r0-basic-reproduction-number-for-a-disease-is-a-fiction-it-does-not-exist-2b389a0478a8
Thanks for your videos! One question about the efficacy of cloth masks
â– Given what we know
1. The covid-19 virus is mainly transmitted in an aerosol form – contained in small droplets of saliva and mucus.
2. The virus is most easily transmitted in cool, dry conditions.
3. The virus is able to survive for at least a few hours on fabric*
â– What happens when the droplets dry out and release the virus particles that they contain?
1. How quickly will the droplets dry out while in the air, especially in dry conditions with low humidity?
2. How long will the virus particles remain suspended in the air and how long might they survive in the air if not exposed to UV light or heat?
3. If separated from the droplets won’t the virus easily flow through most fabric masks or any mask that isn’t designed to trap particles?
4. I understand that cloth masks are often moist from our breath but what happens when the mask and presumably the droplets dry out?
5. If the mask drys out won’t the virus be breathed in through the fabric or expelled into the air since you are breathing through the filter media?
6. Is the virus more or less dangerous when separated from the droplets?
a. Will it survive?
b. Will it remain airborne longer?
d. Will it pass through filters or cloth masks easier?
e. Will it when inhaled be more lethal. For instance in this form is it more likely to bypass our bodies natural defenses such as our cilia, and mucus and more easily reach the ace2 receptors or reach deep into lungs to our alveoli and lodge there or possibly even get into our bloodstream?
* How long the virus will remain a viable seems to be a matter of contention.
▪︎https://nypost.com/2021/02/24/covid-study-finds-virus-survives-on-fabric-for-3-days/
▪︎https://www.news-medical.net/news/20200818/Study-shows-coronavirus-thrives-in-dry-air-with-low-humidity.aspx
â– One final question does smoking affect us getting covid-19 since it relaxes our cilia.