In infectious disease world, the term €œcorrelate of protection€ refers to something that can be measured – antibodies or T cells – which indicates that a person is protected against infection or disease. The correlates of protection for SARS-CoV-2 infection of humans are not yet known – after all it is still early in this pandemic – but many laboratories are investigating whether anti-viral antibodies are the key.
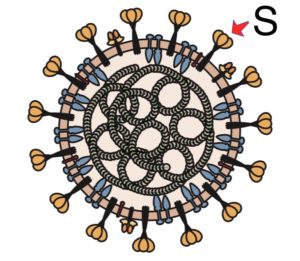
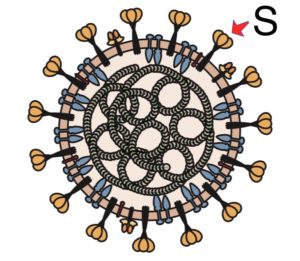
A major assumption of these studies, and indeed of most of the vaccines in development, is that antibodies to the SARS-CoV-2 spike glycoprotein are important for protection. The logic for this is based on several lines of evidence, including the fact that spike binds the cell receptor, ACE2, and so blocking spike prevents infection; and immunization of animals with spike-encoding vaccines, or administration of anti-spike antibodies can prevent infection with SARS-CoV-2 . Vaccine-induced antibodies are clearly a correlate of protection in nonhuman primates. Whether antibodies to spike are protective in humans remains to be determined, but we should have the answer within the year, from the results of vaccine efficacy trials and observing whether natural infection broadly confers protection against reinfection.
Another way to asses the roles of antibodies in protection against COVID-19 is by studying their levels and their durability in patients. Three recent papers have addressed these questions in different ways.
A study of sera from 30,082 individuals with mild to moderate COVID-19 reveals that all have moderate to high titers of antibodies that bind the viral spike protein. The ability of these antibodies to neutralize SARS-CoV-2 infectivity was studied in only 120 samples. While neutralization titers correlated with spike-binding titers, it is not clear if this pattern applies to the entire patient set. Authors report that neutralization titers are stable for at least 5 months, and argue that this longevity is a consequence of long-lived memory B cells in the bone marrow. Whether this assertion is correct must be determined experimentally.
A 3-month study of 65 patients with COVID-19 ranging from asymptomatic to severe also reveals anti-SARS-CoV-2 antibody responses in most patients when sampled beyond 8 days after symptom onset. Neutralizing antibody titers decline within 3 months, often to baseline levels in patients who had less severe disease.
A third study followed 97 non-hospitalized patients for 8 weeks. All produced neutralizing antibodies at different levels which decreased by 45% over 4 weeks.
The results of these studies differ, with the first claiming that anti-SARS-CoV-2 neutralizing antibodies are durable as a consequence of memory B cells, and the other two finding a more rapid decline. Which is correct is not clear as the patient samples and methodologies are different. The question of whether mild to moderate COVID-19 is associated with humoral memory remains an open question. We do know from a recent study that B cell memory is not present in patients with severe disease, as a consequence of lack of germinal centers in lymph nodes and spleen. If B cell memory is established after mild to moderate infection, then reinfection should lead to rapid anti-viral antibody production and possible protection against disease.
Similar studies over longer periods of time are needed to determine if anti-viral antibody levels eventually decline to baseline, implying lack of B cell memory, or if they remain at low levels as they are replenished by long-lived plasma cells in the bone marrow.

Comments are closed.