History
Zika virus was first identified in 1947 in a sentinel monkey that was being used to monitor for the presence of yellow fever virus in the Zika Forest of Uganda. At this time cell lines were not available for studying viruses, so serum from the febrile monkey was inoculated intracerebrally into mice. All the mice became sick, and the virus isolated from their brains was called Zika virus. The same virus was subsequently isolated from Aedes africanus mosquitoes in the Zika forest.
Serological studies done in the 1950s showed that humans carried antibodies against Zika virus, and the virus was isolated from humans in Nigeria in 1968. Subsequent serological studies revealed evidence of infection in other African countries, including Uganda, Tanzania, Egypt, Central African Republic, Sierra Leone, and Gabon, as well as Asia (India, Malaysia, Philippines, Thailand, Vietnam, Indonesia).
Zika virus moved outside of Africa and Asia in 2007 and 2013 with outbreaks in Yap Island and French Polynesia, respectively. The first cases in the Americas were detected in Brazil in May 2015. The virus circulating in Brazil is an Asian genotype, possibly imported during the World Cup of 2014. As of this writing Zika virus has spread to 23 countries in the Americas.
The virus
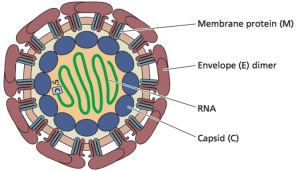
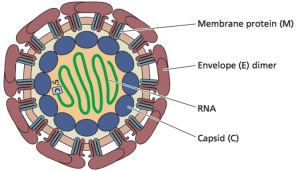
Zika virus is a member of the flavivirus family, which also includes yellow fever virus, dengue virus, Japanese encephalitis virus, and West Nile virus. The genome is a ~10.8 kilobase, positive strand RNA enclosed in a capsid and surrounded by a membrane (illustrated; image copyright ASM Press, 2015). The envelope (E) glycoprotein, embedded in the membrane, allows attachment of the virus particle to the host cell receptor to initiate infection. As for other flaviviruses, antibodies against the E glycoprotein are likely important for protection against infection.
Transmission
Zika virus is transmitted among humans by mosquito bites. The virus has been found in various mosquitoes of the Aedes genus, including Aedes africanus, Aedes apicoargenteus, Aedes leuteocephalus, Aedes aegypti, Aedes vitattus, and Aedes furcifer. Aedes albopictus was identified as the primary vector for Zika virus transmission in the Gabon outbreak of 2007. Whether there are non-human reservoirs for Zika virus has not been established.
Signs and Symptoms
Most individuals infected with Zika virus experience mild or no symptoms. About 25% of infected people develop symptoms 2-10 days after infection, including rash, fever, joint pain, red eyes, and headache. Recovery is usually complete and fatalities are rare.
Two conditions associated with Zika virus infection have made the outbreak potentially more serious. The first is development of Guillain-Barre syndrome, which is progressive muscle weakness due to damage of the peripheral nervous system. The association of Guillain-Barre was first noted in French Polynesia during a 2013 outbreak.
Congenital microcephaly has been associated with Zika virus infection in Brazil. While there are other causes of microcephaly, there has been a surge in the number of cases during the Zika virus outbreak in that country. Whether or not Zika virus infection is responsible for this birth defect is not known. One report has questioned the surge in microcephaly, suggesting that it is largely attributed to an ‘awareness’ effect. Current epidemiological data are insufficient to prove a link of microcephaly with Zika virus infection. Needed are studies in which pregnant women are monitored to see if Zika virus infection leads to microcephaly.
Given the serious nature of Guillain-Barre and microcephaly, it is prudent for pregnant women to either avoid travel to areas that are endemic for Zika virus infection, or to take measures to reduce exposure to mosquitoes.
Control
There are currently no antiviral drugs or vaccines that can be used to treat or prevent infection with Zika virus. We do have a safe and effective vaccine against another flavivirus, yellow fever virus. Substituting the gene encoding the yellow fever E glycoprotein with that from Zika virus might be a good approach to quickly making a Zika vaccine. However testing of such a vaccine candidate might require several years.
Mosquito control is the only option for restricting Zika virus infection. Measures such as wearing clothes that cover much of the body, sleeping under a bed net, and making sure that breeding sites for mosquitoes (standing water in pots and used tires) are eliminated are examples. Reducing mosquito populations with insecticides may also help to reduce the risk of infection.
Closing thoughts
It is not surprising that Zika virus has spread extensively throughout the Americas. This area not only harbors mosquito species that can transmit the virus, but there is little population immunity to infection. Infections are likely to continue in these areas, hence it is important to determine whether or not Zika virus infection has serious consequences.
Recently Zika virus was identified in multiple states, including Texas, New York, and New Jersey, in international travelers returning to the US . Such isolations are likely to continue as long as infections occur elsewhere. Whether or not the virus becomes established in the US is a matter of conjecture. West Nile virus, which is spread by culecine mosquitoes, entered the US in 1999 and rapidly spread across the country. In contrast, Dengue virus, which is spread by Aedes mosquitoes, has not become endemic in the US.
We recently discussed Zika virus on episode #368 of the science show This Week in Virology. You can be sure that we will revisit this topic very soon.
Added 1/28/16 9:30 PM: The letter below to TWiV provides more detail on the situation in Brazil.
Esper writes:
Hi TWIVomics
I hope this email finds you all well and free of pathogenic viruses.
My name is Esper Kallas, an ID specialist and Professor at the Division of Clinical Immunology and Allergy, University of São Paulo, Brazil.
I have been addicted to TWIV since a friend from U. Wisconsin participated in the GBV-C episode (David O’Connor, episode #260). Since then, never missed one episode. After long silent listening, I decided to write for the first time, motivated by the ongoing events in my country, potentially related to the Zika virus.
In the last episode, Emma wrote about events taking place in the small town of Itapetim, State of Pernambuco, Northeastern Brazil, which I will describe a bit later in this email. Before, let me bring some background information on the current situation.
Most believed Zika was a largely benign virus, causing a self-limited disease, clearly described in episode #368. Its circulation was documented after an outbreak became noticed in the State of Bahia (NE Brazil) by a group led by Guilherme Ribeiro, a talented young Infectious Diseases Scientist from Fiocruz (PMID: 26584464, Emerg Infect Dis. 2015 Dec;21(12):2274-6, free access)
However, things started to get awkward around October 2015, when a single hospital in Recife (NE Brazil) and some other practicing Obstetricians and Pediatricians from the region started reporting a mounting number of microcephaly cases in newborns, later confirmed by the national registry of newborns. The numbers are astonishing. The graph below depicts the number of cases per year prior to the surge in 2015. Only this year, 2,975 cases were reported by December 26, the vast majority in the second semester of the year. Cases are concentrated in the Northeast (map), with 2,608 cases, including 40 stillbirths or short living newborns.


In response to the situation, the Brazilian Ministry of Health has declared a national public health emergency (http://portalsaude.saude.gov.br/index.php/cidadao/principal/agenciasaude/20629-ministerio-da-saude-investiga-aumento-de-casos-de-microcefalia-em-pernambuco).
The Brazilian Ministry of Health has been presenting updates every week (see link: http://portalsaude.saude.gov.br/index.php/o-ministerio/principal/leia-mais-o-ministerio/197-secretaria-svs/20799-microcefalia). It is important to observe some imperfections in these numbers: 1. There may be an over reporting after the news made to the big media, suggesting an association between microcephaly and Zika virus. 2. The criterion to consider a microcephaly case has been changed after the current epidemic from 33cm to 32cm; this is because 33cm of head circumference is sitting in the 10th percentile of newborns at 40 weeks of pregnancy and the adjustment would bring the limit to the 3rd percentile, increasing the specificity to detect a true microcephaly case (this may result in an over reporting in the beginning of the epidemic).
The association between Zika virus infection and microcephaly was suspected since the beginning, when Brazilian health authorities ruled out other potential causes, together with the fact that the microcephaly epidemic followed Zika virus spread. Further evidences were the two positive RT-PCR for Zika RNA in two amniotic fluids obtained from two pregnancies of microcephalic fetuses and a stillborn microcephaly case with positive tissues for Zika RNA. In fact, French Polynesia went back to their records and also noticed an increase of microcephaly case reporting, following their epidemic by the same virus strain in 2013 and 2014.
Now, Zika virus transmission has been detected in several countries in the Americas (http://www.paho.org/hq/index.php?option=com_topics&view=article&id=427&Itemid=41484&lang=en).
Although strong epidemiological data suggest the association between Zika virus and the microcephaly epidemic, a causal link between the virus and the disease is still lacking and is limited to few case reports. Many questions still remain. Does the virus damage embryonic neural tissue? What is the percentage of fetuses getting infected when the mother acquires Zika virus during pregnancy? Does the stage of pregnancy interfere with virus ability to be transmitted to the fetus and the development of neurologic effects? Are there other neurological defects related to Zika virus infection? Is there another cofactor involved, such as malnutrition or other concurrent infection? All these questions are exceedingly important to provide counseling to pregnant women and those who are planning to become pregnant, especially in Northeastern Brazil. In fact, Brazilian authorities have been recommending avoiding pregnancy until this situation is further clarified.
The microcephaly epidemic impact is unimaginable. It is a tragedy. These children are compromised for life and the impact on their families is beyond any prediction.
Back to the story sent by Emma. A small town in the North of Pernambuco State, named Itapetim, has almost 14 thousand inhabitants and has reported 11 cases of microcephaly in the past 3 months. This very same town has been suffering from a prolonged drought, since September 2013 when the last reservoir went dry. Perhaps the storage of clean water or the limited resources has led to the best environment for arbovirus spread and the development of microcephaly.
But the Zika virus’s impact may be reaching further. An increase in Guillain-Barre syndrome cases has also been noticed in the Northeast of Brazil, possibly related to the epidemic.
Several groups have been trying to establish animal models to study the interaction of Zika virus with neural tissue. The forthcoming developments are critical to better understand the virus immunopathology and confirm (or refute) the association between the virus infection and neurologic damage in fetuses and in the infected host developing Guillain-Barre syndrome. Many things still shrouded in mystery.
Keep on the good work. I will keep on listening!
Esper

Thank you for the information! I am a student within the field of arts in medicine/arts in health, and have been doing a small amount of research out of personal curiosity on the correlation between Zika and cases of Guillain-Barré syndrome in patients. Given the distinct connection between Zika and an increase in cases of Guillain-Barré syndrome, in patients who have suffered severe paralysis, do you think that there could be a benefit to engaging patients in artistic rehabilitation exercises during their recovery process? My thoughts are that in conjunction with the specialties of a nurse or occupational therapist, that patients experiencing paralysis of their arms and hands might strongly benefit from engaging in making art, and perhaps even speed up the recovery process in gaining back some dexterity that has been temporarily lost due to the effects Guillain-Barré syndrome. I would love to know your thoughts on this, or to hear if anyone knows of any arts-based research that is being conducted in this focus.
I was not aware of how long Zika has been known for. As a resident of Miami, Florida, I am well aware of the Zika virus and the affects it has on people, especially pregnant women. It brings major concern to me that Zika can cause congenital microcephaly and even Guillain-Barré syndrome. It is imperative that a vaccine be invented, but this can take several years to do. The CDC must try to collect enough funds in order to create a vaccine in the near future. More research should also be performed. For now I think it is extremely important to spread the word about Zika and learn preventative measures from contracting the virus. It is vital the pregnant women are aware of this. It should be discussed in OB/GYN clinics. In certain areas where Zika was dense in Miami, city officials went around that area handing out mosquito repellant to the public. Other areas with the mosquitos that carry Zika should do this as well.
Pingback: Zika virus was first identified in 1947 in a sentinel monkey that was being used to monitor for the presence of yellow fever virus in the Zika Forest of Uganda. – Vaccine Common Sense