Primary influenza virus infection increases colonization of the human upper and lower respiratory tract with bacteria, including Streptococcus pneumoniae and Staphylococcus aureus. Such infections may lead to complications of influenza, including pneumonia, bacteria in the blood, sinusitis, and ear infections.
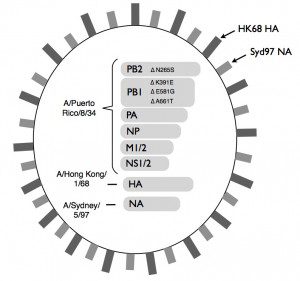
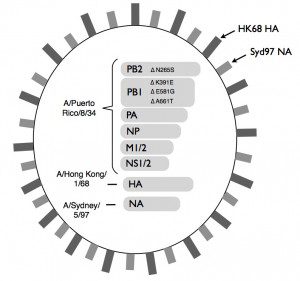
One of the vaccines available to prevent influenza is an infectious, attenuated preparation called Flumist. To determine if a vaccine such as Flumist increases susceptibility to bacterial infection, the authors created their own version of the vaccine (illustrated) in which the six RNA segments encoding internal proteins were derived from the A/Puerto Rico/8/34 (H1N1) strain (allowing replication in mice), and the HA and NA proteins were derived from A/Hong Kong/1/68 (H3N2). In addition, mutations were introduced into the viral genome that are important for the safe and protective properties of Flumist. For simplicity we’ll call this virus ‘live attenuated influenza virus’, or LAIV.
Mice were inoculated intranasally with a strain of S. pneumoniae known to colonize the nasopharynx, followed 7 days later by LAIV or wild type influenza virus. Inoculation with either virus similarly increased the bacterial levels in the nasopharynx, and extended the time of colonization from 35 to 57 days. In mice that were given only bacteria and no influenza virus, the inoculated bacteria were cleared beginning 4 days after administration. The more extensive and extended colonization of virus-infected mice was not associated with overt disease.
Administration of LAIV or wild type virus 7 days before bacteria also resulted in excess bacterial growth in mice. Similar results were obtained using S. aureus. Administration of S. pneumoniae up to 28 days after virus also lead to excess bacterial growth, despite clearance of the viruses around 7 days after vaccination.
All mice died when they were vaccinated with wild type influenza virus followed 7 days later by a sublethal dose of a highly invasive strain of S. pneumoniae. In contrast, pretreatment with LAIV lead to no disease or death of any mice.
It is not known if these findings in a mouse model directly apply to humans. However, because Flumist reduces influenza virus replication, it is associated with a decrease in secondary bacterial infections. It is possible that, after administration of LAIV to humans, there is an increase in bacterial colonization of the respiratory tract. Upper respiratory tract symptoms are a known adverse effect of LAIV, and it is possible that these might be related to increased bacterial loads. It is important to emphasize that use of LAIV is not associated with severe upper or lower tract disease.
These findings are important because they show that a mouse model could be used to understand why influenza virus infection leads to increased bacterial colonization of the respiratory tract. It will be important to determine the precise mechanisms by which influenza virus infection, and the associated virus and immune-mediated alteration to the respiratory tract, allows enhanced bacterial colonization. At least one mechanism, which we discussed on episode #62 of This Week in Microbiology, involves the disruption of biofilms, allowing bacteria to enter the bloodstream.

Pingback: Attenuated influenza vaccine enhances bacterial...
does this increased colonization with bacteria induce longlasting
immunity to those ? Like a bacterial vaccine.
And could age-dependent acquired bacterial immunity following bacterial infection following
influenza infection in the 1889 pandemic be the reason for the unusual age-death-curve
in 1918 ?