Vaccines work by educating the host’s immune system to recall the identity of a virus years after the initial encounter, a phenomenon called immune memory. Viral vaccines establish immunity and memory without the pathogenic consequences typical of a natural infection. The success of immunization in stimulating long-lived immune memory is among humanity’s greatest scientific and medical achievements.
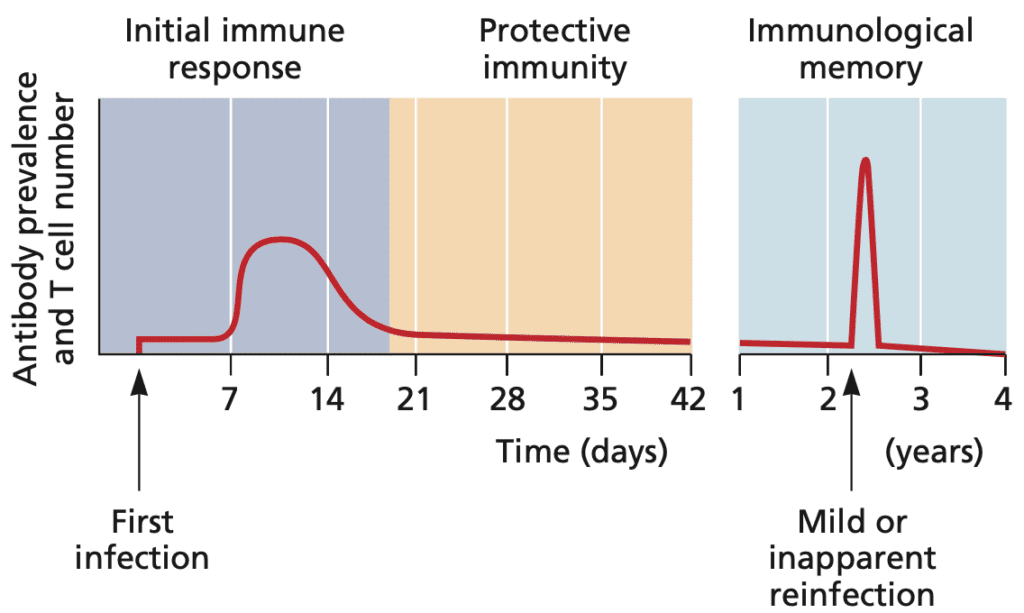
Immune memory is maintained by dedicated T and B lymphocytes that remain after an infection has been resolved, and most activated immune cells have died. These memory cells can respond rapidly to a subsequent infection (Figure). Ideally, an effective and durable vaccine is one that induces and maintains significant numbers of memory cells. If the host is infected again with this same pathogen, the memory B and T cells initiate a response that rapidly controls the pathogen before disease develops. This paradigm is true for most human viruses for which vaccines exist, including measles, mumps, and varicella-zoster viruses and poliovirus. In some cases, antigenic variation, such as occurs with influenza virus, precludes complete protection by a memory immune response, necessitating re-vaccination.
Protection from Infection or Protection from Disease?
The memory response elicited by most human viral vaccines does not protect against reinfection, but rather against the development of disease. An individual may be exposed repeatedly to viruses and never be aware of it, because the memory response eliminates the virus before signs and symptoms develop. After vaccination with inactivated poliovirus vaccine, virus replication may take place in the intestine, but effectively blocks the development of poliomyelitis. On the other hand, the human papillomavirus vaccine is over 90% effective at blocking infection. Consequently the HPV vaccine induces sterilizing immunity.
Whether or not COVID-19 vaccines will block infection is unknown because it has not been adequately measured. The results of a few small studies suggest that some of the vaccines may prevent infection. However these studies are not conclusive because they are being done shortly after vaccination, when serum antibody levels are much higher than they will be in, say, 6 months. Only then will we have an accurate measure of how well vaccination blocks infection with SARS-CoV-2. I suspect that none of the COVID-19 vaccines will block infection, but will reduce virus reproduction sufficiently to impede transmission in the population.
Population-wide immunity (aka herd immunity)
To be effective, a vaccine must induce protective immunity in a significant fraction of the population. Not every individual in the population need be immunized to stop viral spread, but the number must be sufficiently high to impede virus transmission. Person-to-person transmission stops when the probability of infection drops below a critical threshold. This effect is called herd immunity.
The herd immunity threshold is calculated as 1- 1/R0. R0 is the number of nonimmune individuals that on average will be infected upon encounter with an actively infected individual. As the reproduction number, R0, increases the value of 1/R0 decreases, and thus 1 ˆ’ 1/R0 gets closer to 1, or 100%. For smallpox virus, the herd immunity threshold is 80 to 85%, while for measles virus (which has a high R0), it is 93 to 95%. Early in the COVID-19 outbreak the R0 of SARS-CoV-2 was calculated to be 2-3, which would produce a herd immunity threshold of 50-70%.
Herd immunity only works when a vaccine either blocks infection, or sufficiently reduces virus reproduction in the host to impede person to person transmission. As stated above, I see no reason why COVID-19 vaccines will not sufficiently reduce transmission to enable herd immunity.
No vaccine is 100% effective at inducing immunity in a population. Consequently, the level of immunity is not equal to the number of people immunized. For example, when 80% of a population is immunized with measles vaccine, about 76% of the population is actually immune, well below the 93 to 95% required for herd immunity.
What about T cells?
For many virus infections, antibodies are crucial for preventing infection. However, resolution of infection often requires the action of cytotoxic T cells, which kill virus infected cells. For vaccines that do not induce sterilizing immunity, it is likely that T cells play a role in eliminating virus-infected cells and preventing the development of disease.
This division of labor has been largely ignored in the discussion of COVID-19 vaccines. Most of the dialog has concerned the induction of antibodies and their ability to neutralize virus infection. COVID-19 vaccines do induce virus-specific T cells and it is likely that these will clear infections that begin in vaccinated indivduals. It has been reported that amino acid changes in SARS-CoV-2 variants of concern do not affect T cell epitopes, and that T cell responses in individuals who have either recovered from infection or have been vaccinated are not affected by these changes. Therefore it seems likely that even if variants of concern are able to overcome to some degree previous antibody immunity, they will be cleared by T cell responses, avoiding severe disease and death. The results of the phase III trial of the J&J COVID-19 vaccine support this presumption.

Clear, concise, and to the point. Thanks.
Will the Covid vaccine be deemed a “leaky” one in the future, with disastrous consequences like what happened with Marek’s disease?
Pingback: How vaccines work - Virology Hub
Melodine seems to have wandered over from the magic shop.
“ And if the dam breaks open many years too soon
And if there is no room upon the hill
And if your head explodes with dark forebodings too
I’ll see you on the dark side of the moonâ€