A super spreader is an individual who is more likely to infect others compared with a typical patient (pictured). An example is the doctor who treated early SARS-CoV patients in China, traveled to a hotel in Hong Kong, and infected 10 others who then went on bring the virus to multiple countries. Superspreaders of SARS-CoV-2 have been thought to be involved in transmission of the virus and the results of a recent study confirm their substantial role in the pandemic.
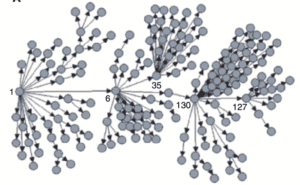
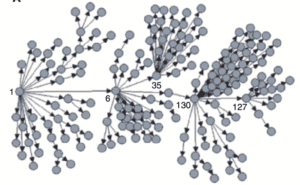
Analysis of superspreaders was done by examining 1,038 confirmed cases in Hong Kong up to 28 April. Over half of these infections were associated with at least one of 137 clusters (two or more confirmed cases). The median size of a cluster was 2 cases and the largest had 106 cases. Some 41% of the cluster cases were initiated locally, and 16% were initiated by an imported case. However, most clusters (63%) were initiated overseas. Of the 505 cases that were not linked to clusters, over 90% were acquired overseas. Transmission in social settings (bars, weddings) was linked to more secondary cases than households. Parenthetically, 19% of all cases in Hong Kong were asymptomatic at confirmation.
The largest cluster (106 cases) was traced to four bars in Hong Kong and was spread in part by musicians traveling between the venues. This cluster contained one or more superspreader events. The second largest cluster (22 cases) was linked to two superspreader events at a wedding and a preceding social event. The third largest cluster (19 cases) was linked to attendance at a temple with 12 cases part of a superspreader event. An asymptomatic monk who worked at the temple was likely the source of 11 temple cases.
These data were used to calculate the reproduction number R. The basic R0 of SARS-CoV-2, calculated early during the outbreak in Wuhan, is 2-3. The reproductive number calculated from the Hong Kong data is 0.62, a reflection of quarantine and isolation measures put in place during the outbreak. The dispersion coefficient was determined to be 0.35. The latter number indicates that 19% of cases were responsible for 80% of all SARS-CoV-2 transmission. Remarkably, 69% of cases did not transmit to anyone. These conclusions are in line with observations made in other countries.
Those conclusions need to be repeated: 19% of cases were responsible for 80% of all SARS-CoV-2 transmission, and 69% of cases did not transmit to anyone.
Wouldn’t it be great if we could identify the superspreaders, quarantine them, and stop 80% of all transmission? Right now we can’t. But what we can do is isolate confirmed cases very quickly. In Hong Kong, the median time from onset of symptoms to lab confirmation was 6 days for transmitters. That’s too long: onward transmission has likely already occurred in 6 days. Confirmation and isolation has to occur VERY quickly.
Based on these data, the authors suggest the following disease control measures:
€¢Rapid tracing and quarantine of confirmed contacts
€¢Physical distancing
€¢Closure or reduced capacity measures of high risk social settings (bars, weddings, religious sites, restaurants)
America, do you understand, or will some of you continue to ignore reality?

Pingback: Superspreaders of SARS-CoV-2 - Virology Hub
In the UK, the ‘powers that be’ seem to think that the virus can’t be spread via postal letters and parcels. People are given advice to that effect on information bites that come up frequently on Sky News. Is this true? I seem to remember that a study done earlier in the outbreak showed that the virus could last for a day or more on cardboard, so wouldn’t it be sensible to advise people to leave their mail for a day or longer before touching it and to remind them to wash their hands and any contact surfaces thoroughly when they do? I appreciate that the risk may be lower than with other surfaces, but if a postman/woman or sorting office/distribution worker was a super spreader then surely a lot of people could be put at risk?
Is there any data (or can we extrapolate from anything we already know) about whether being a superspreader is a product of biology (some people are just inherently superspreaders), behavior (if you do X or Y, you’re likely to become a superspreader), or some combination of the two (I imagine it’s the latter, but I wonder what the ratio is)?
CT asked about SARS CoV-2 stability on surfaces. TWIV 591 contains a discussion and link to a paper by Munster that answers your question. Yes, surfaces are a risk but evidence suggests infections are largely airborne sourced.
https://www.microbe.tv/twiv/twiv-591/
What’s happening with religious sites are that if you go and keep all protocoles ther is nomuch risk.we stand in 2m distance wearing masks ,use.a sanitizer while register in ledger .keeps chappal at 2m away outside in the courtyard
.problem is that people go and mingle each other after church time .this is what really causing spread.
I will like to know if there is information regarding mother and child transmission during pregnancy or delivery?
Any data on demographics of super spreaders? gender? age? etc