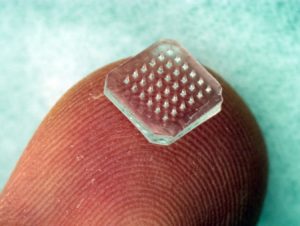
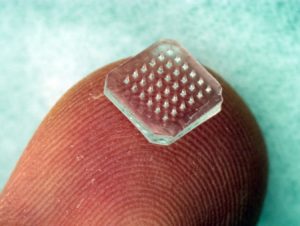
Most of the 172 SARS-CoV-2 vaccines in development will be administered by intramuscular injection, a traditional route for many effective vaccines. In my opinion the use of needles for immunization will one day be replaced by microneedle patches, which can not only be self-administered but have a variety of other advantages compared with injection.
A microneedle patch is fabricated with a plastic containing the vaccine antigen. When applied to the skin with a band-aid, the needles pass through the dead upper layers of skin and into the underlying dermis and epidermis. The latter is rich in antigen presenting and accessory cells of the immune system, an environment that favors potent and durable adaptive immunity. The needles dissolve in the skin, releasing antigen. The release of antigen is a small area increases vaccine concentration while reducing the dose used compared with injection. Afterwards the patch, which is no longer sharp, is discarded in normal trash.
Immunization via microneedle patch does not require a trained health care worker, an obvious advantage which saves money and allows deployment in resource challenged areas. Furthermore, incorporation of antigen into the plastic matrix appears to confer thermal stability, eliminating the need for a cold chain.
A variety of microneedle based vaccine candidates for viruses, bacteria, and protozoan parasites have been formulated and tested in experimental animals and in humans. The latest is a vaccine candidate for SARS-CoV-2; the results demonstrate that this platform is suitable for use in rapidly developing vaccines against emerging pathogens.
Within 3 weeks of publication of the genome sequence of SARS-CoV-2, the gene for the spike glycoprotein was synthesized and inserted into mammalian cells in culture. The recombinant spike protein was purified and microneedle patches were fabricated using molds filled with carboxymethyl cellulose mixed with antigen.
Microneedle patches were applied to the skin of mice and sera were collected at different times afterwards. High levels of virus-specific IgG was detected by week 2. Sterilization of the patches by gamma-irradiation did not compromise immunogenicity.
The next step is to determine whether the antibodies induced by microneedle patch immunization can neutralize SARS-CoV-2 infectivity. If they do, with the proper preclinical data this vaccine candidate can proceed to human clinical trials. Given the many advantages of microneedle patches compared with needle-based immunization, I am hopeful that they will be one of the vaccines that are approved and used to prevent COVID-19. Such use would validate microneedle patches as a vaccine platform and enable their use for future emerging viruses.
Of course, kids (and their parents) will love microneedle patches – they don’t hurt!

Pingback: Microneedle patch SARS-CoV-2 vaccine candidate – Virology Hub
I love this one! Microneedle patches seem so easy that it would be a shame if they do not work in humans the way they work in mice. The problem with the microneedle patches with SARS-CoV-2 spike protein antigen in them is that the virus is constantly mutating, and today’s patch antigen may differ from tomorrow’s spike protein. For a remedy for COVID-19 (not a vaccine) that won’t become obsolete because it targets the viral RNA polymerase, I offer this: “Take a scant tsp of CsCl in a glass of juice, wait ~8 hr, then eat a banana. Prepare for heavy diarrhea. Repeat no more than 3-4 times.” That’s it!