Timothy Ray Brown, also known as the Berlin patient (reviewed in a previous post), was the only person ever to be cured of HIV/AIDS. Until last week.
In a report published in the journal Nature, a group of investigators announced the cure of a second HIV-positive patient (designated the “London patient”). In the context of HIV infection, the term “cure” means the complete elimination of all virus-carrying cells. Standard antiretroviral therapy (ART) is very effective at reducing the viral load in the blood of infected individuals and preventing transmission to others. However, it does not eliminate all infected cells, allowing the persistence of a small pool of cells collectively known as the HIV reservoir. If ART is interrupted or terminated, the virus will begin replicating again within a couple of weeks because of this reservoir.
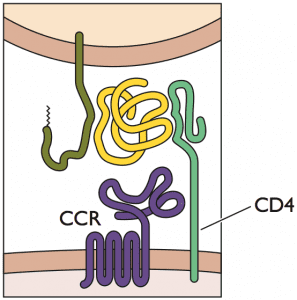
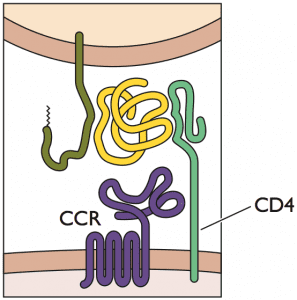
Timothy Ray Brown and the London patient shared similar medical circumstances. They were both HIV-1-positive and receiving ART therapy. They both eventually developed a blood cancer (acute myeloid leukemia and Hodgkin’s lymphoma, respectively), which was treated with chemotherapy and various other therapeutics. Both ultimately required a bone marrow transplant to replenish the blood stem cells that had been destroyed during chemotherapy. In both cases, doctors used bone marrow cells from a donor who was homozygous for a mutation in the gene encoding the HIV co-receptor CCR5 (CCR5 Δ32/Δ32), because this genotype confers resistance to HIV-1 infection. Both patients were cured of their cancer. As hoped, both patients were also cured of their HIV infection, as evidenced by the absence of virus in their blood many months after termination of ART.
Both patients also experienced mild cases of graft-versus-host disease, a condition in which residual white blood cells in the donated sample recognize the recipient as non-self and attack the recipient’s cells. It is possible that this condition contributed to the complete loss of HIV-infected cells. Because both patients also reached and maintained full donor chimerism (meaning that their post-transplant hematopoietic cells were all of donor origin), their reservoir size may have been drastically reduced or even completely eliminated.
Before receiving bone marrow from a donor, patients undergo what is known as a conditioning regimen. This regimen typically consists of chemotherapy, total body irradiation, or a combination thereof, and it serves to kill any residual cancer cells, suppress the immune system so it won’t reject the new bone marrow cells, and clear space for the donor cells to grow. It is possible that this conditioning regimen also contributed to the destruction of cell reservoirs that harbor HIV.
One difference between the treatment processes for the two patients was that Brown’s treatment regimen was considerably more invasive. Brown experienced a relapse of his cancer after his first transplant, necessitating a second transplant. Each of his transplants was preceded by an aggressive conditioning regimen of immunosuppressive drugs and total body irradiation. The collective trauma of these procedures was immense; he experienced delirium, temporary blindness, and paralysis. To recover, he had to be placed in a medically induced coma and he almost died. In contrast, the London patient’s cancer went into full remission after just one bone marrow transplant. His conditioning regimen was also notably milder and did not include irradiation. It has now been 18 months since he stopped ART and he is still virus-free.
While these two cases have provided important insight for HIV research, they are not exactly a breakthrough in the search for a cure. It’s important to consider that both of these patients needed the bone marrow transplant because they had cancer. Bone marrow transplantation is a very risky procedure with a roughly 50% chance of success and hence not a feasible strategy to cure HIV infection. A preferable approach for a cure would involve modifying a patient’s CCR5 receptor using newly available gene editing technology, without the need for a bone marrow transplant. Until scientists are able to achieve this goal, standard ART regimen is still the best treatment option, because it is highly effective in preventing transmission and it allows for near normal life expectancy.
[The material in this blog post is also covered in episode 28 of Catch This.]

Pingback: The London Patient – Virology Hub
Pingback: The London Patient -
As I have commented before, without the comment gaining much traction, HIV-1 has an alternate reservoir location besides blood cells: it also resides in astrocytes in the brain. In astrocyes, HIV-1 expression is limited to NEF and perhaps other accessory proteins “restricted infection”, so encapsidated, infectious virus is not produced, and immune surveillance is avoided. However, the virus is still there, waiting to be reactivated. I am happy for the two HIV-1 infected individuals whose virus was thought to have been eliminated by blood cell replacement in the course of cancer chemotherapy, but I continue to caution that unless they also undergo astrocyte replacement, an impossibility, some residual HIV-1 will remain.