by Gertrud U. Rey
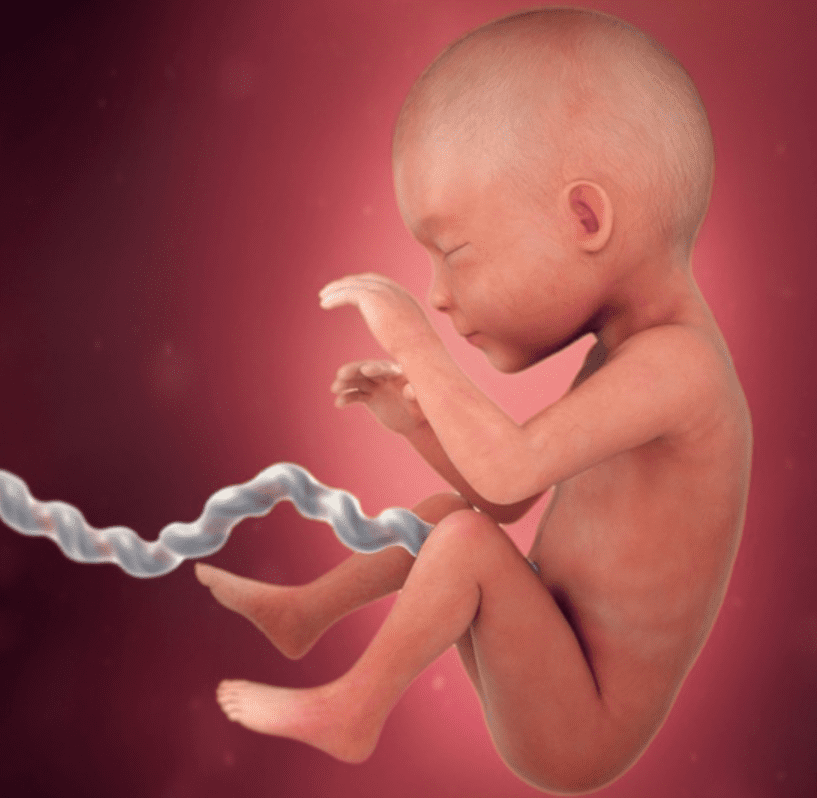
During the first few months of life, residual maternal antibodies that crossed the placenta during gestation and antibodies from breast milk protect infants from infection with various microbes. This type of immune protection is known as “passive immunity,” and differs from “active immunity,” which develops in an individual following vaccination or natural infection with a pathogen.
Active immunity involves the function of both antibodies and T cells. During a first exposure to a pathogen (or immunization against that pathogen), T helper cells sense the presence of one or more antigens as foreign and trigger the release of a variety of signals that ultimately stimulate B cells to secrete antibodies to those antigens. T helper cells also stimulate cytotoxic T cells to directly kill infected target cells. This initial immune response can take weeks to develop. However, exposure to the same antigen months or years later leads to a rapid immunological memory reaction that results in production of new antibodies and T cells.
In contrast, passive immunity is limited to the action of antibodies that are acquired from an external source. As mentioned above, a notable example of passive immunity involves the antibodies an infant receives from its mother. However, passive immunity can also be acquired through intravenous infusion of convalescent plasma from a person who has recovered from an infection, or through infusion of monoclonal antibodies against a particular pathogen. Monoclonal antibodies are made in the lab, are derived from a single B cell lineage (i.e., a single clone), and are very effective at eliminating unwanted antigens or cells. Although the effects of passive immunity are immediate, they only last a few weeks or months because they are limited to the input number and lifespan of the acquired antibodies. Passive immunity also does not give rise to any immune memory, meaning that the immune system will respond to a subsequent infection with the same pathogen as if it were an initial infection, which is a less efficient and more time-consuming process than if the endogenous immune system has previously seen the pathogen.
Passive immunity and active immunization often overlap and can interfere with each other in a phenomenon known as immune blunting. For instance, circulating maternal anti-measles virus antibodies can prevent an infant’s B cells from producing its own antibodies in response to measles vaccination or infection with measles virus. A recent epidemiological study on the dynamics of measles immunity showed that maternal anti-measles virus antibodies have a half-life of 181 days. Because such antibodies can block the infant’s ability to produce anti-measles antibodies, administration of the first dose of the measles vaccine prior to 12 months of age may not result in optimal vaccine-induced antibody concentrations. Epidemiological data from China, where the first dose of the measles vaccine is given at eight months of age, have substantiated this presumption – about a third of the individuals who developed measles between 2013 and 2019 had been vaccinated. It is therefore conceivable that some infants didn’t develop an effective immune response to the vaccine because at the time of vaccination these individuals still had circulating maternal antibodies that interfered with the effects of the vaccine, i.e., immune blunting had occurred. These data also confirm that measles vaccination at or after 12 months (as is done in the US and many other countries) may result in longer-lasting immune protection.
Immune blunting was also observed during the COVID-19 pandemic, when recipients of convalescent plasma or monoclonal antibodies developed inferior immune responses to COVID-19 vaccines if they were vaccinated within 90 days after the passive immune treatment. In other words, residual circulating anti-SARS-CoV-2 antibodies from their treatment with convalescent plasma or monoclonal antibodies likely attacked the vaccine antigen before their B cells had a chance to form their own antibodies, thus diminishing the efficacy of the vaccine.
More studies are needed to evaluate the kinetics of passive immunity against various pathogens. Understanding the variability of maternal antibody concentrations in different infants could inspire better strategies for minimizing the risk of immune blunting; and could also lead to more informed vaccine policies.
[The paper linked above was discussed on TWiV 1117. The material in this blog post is also covered in Catch This Episode 61.] ]
