by Gertrud U. Rey
There is still no real cure for HIV infection. Only two people have been intentionally and successfully cleared of the virus thus far – the Berlin patient and the London patient. However, both subjects needed dangerous stem cell transplants to replenish their blood stem cells that had been destroyed during chemotherapy regimens needed to treat their HIV-induced blood cancers. In their transplants, doctors used bone marrow cells from a donor who was homozygous for a mutation in the gene encoding the HIV co-receptor CCR5 (CCR5 Δ32/Δ32), because this genotype confers resistance to HIV-1 infection. Such a transplant strategy cannot be realistically applied to most HIV patients.
Recently, a thirty-year-old female resident of Esperanza, Argentina, was declared to be cured of HIV-1 without receiving long-term treatment. The “Esperanza patient” is actually the second individual known to have cleared the infection naturally. The first person, known as the “San Francisco patient,” is a 67-year-old woman who appears to have cleared the virus in the absence of treatment after living with HIV for 28 years. Standard HIV treatment involves a combination of drugs known as antiretroviral therapy (ART), which is very effective at reducing the viral load in the blood of infected individuals and preventing transmission to others. However, ART does not eliminate all infected cells, allowing the persistence of a small pool of cells collectively known as the HIV reservoir. If ART is interrupted or terminated, the virus will begin replicating again within a couple of weeks because of this reservoir. The reservoir cells are capable of clonally expanding, and surprisingly, not all offspring of a clone exhibit identical levels of viral expression. Developing effective strategies to identify and eliminate such pools of cells is a prevailing challenge in the HIV field. Even the small group of HIV-infected individuals known as “elite controllers” who are able to maintain suppressed viral levels without ART retain a low frequency of intact integrated HIV DNA copies known as proviruses in their peripheral T helper cells.
The Esperanza patient was determined to be an elite controller because she had a very low viral load and no clinical or laboratory signs of HIV-1-associated disease for the entire eight years following her diagnosis, despite receiving no ART during that time. She only underwent ART when she became pregnant, but discontinued treatment after giving birth. To determine whether she had a persistent HIV-1 reservoir, the authors of a recent publication collected blood samples and placental tissue from the patient. They then isolated ~1.2 billion peripheral blood cells and ~0.5 million placental cells from the samples and subjected the cells to amplification and sequencing using primers and probes specific for HIV-1 in a technique that detects single, near full-length HIV-1 proviral genomes. The authors only detected seven proviral HIV-1 DNA species in the blood cells and none in the placenta. However, each of the seven HIV-1 DNA species was defective: one near-full-length sequence contained mutations that were lethal for the virus, and the other six sequences each contained large deletions. Three of these six sequences with deletions were completely identical to each other, suggesting that they were products of clonal expansion. These results distinguished the patient from other elite controllers, indicating that even though she had been infected with HIV-1 at some point and viral replication had occurred in the past, all viral DNA resulting from recent replication cycles was damaged.
The patient’s peripheral blood cells were also used to isolate 150 million T helper cells, which are the primary target of HIV-1. When the authors analyzed these T cells for the presence of replication-competent HIV-1 particles, they did not detect a single virion, a feature that further distinguished the Esperanza patient from other elite controllers, whose blood typically contains up to 50 replication-competent virions per milliliter.
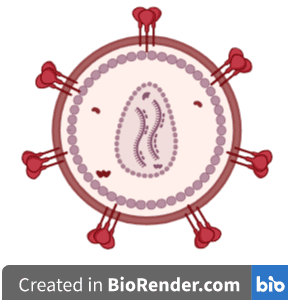
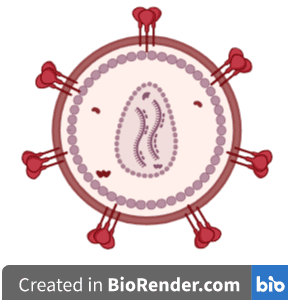
The entry of HIV-1 into cells requires the presence of two cell surface proteins: the receptor CD4, and one of two co-receptors, either CXCR4 or CCR5. Individuals with a CCR5 Δ32/Δ32 genotype, which signifies a mutation in both copies of the gene encoding CCR5, are resistant to HIV-1 infection. Analysis of T helper cells isolated from the Esperanza patient revealed that they fully expressed both wild-type versions of CCR5 and CXCR4 co-receptors, and when tested in vitro, these cells were able to support HIV-1 infection and replication. This observation suggests that the patient was not resistant to infection. However, her serum did not contain the entire antibody profile usually found in HIV-1-positive patients, implying that even though she became infected and replicated virus, she never developed a full HIV-1-specific antibody response.
The complete elimination of all virus-carrying cells in the context of HIV infection is termed a “sterilizing cure,” and the mechanism responsible for this exceedingly rare phenomenon is unclear. The human immune proteins APOBEC3G and APOBEC3F are known to induce destructive nucleotide changes in the HIV genome, and the authors hypothesize that the lethal mutations found in the near full-length HIV-1 proviral sequence were likely induced by these immune proteins. However, it is unclear why the overall number of proviral species was so low.
Whether or not the Esperanza patient will remain permanently free of HIV is currently unclear. The authors are careful to note that “absence of evidence for intact HIV-1 proviruses in large numbers of cells is not evidence of absence of intact HIV-1 proviruses.” Nevertheless, this study suggests that a sterilizing cure of HIV-1 infection is possible, even if it is rare. The authors hope that additional data collected from the San Francisco and Esperanza patients will provide further insight into the mechanism responsible for a sterilizing cure, which might lead to treatments that cause the immune system to mimic the responses observed in these two patients.
[This article was written in honor of World AIDS Day, which occurs annually on December 1. The material in this blog post is also covered in episode 28 of Catch This.]

Pingback: The Esperanza Affected person | News I Can
Pingback: Virology Hub - All about viruses of human, animals and plants
This erudite author continues to miss the main reason why HIV-1 is so difficult to completely eliminate: HIV-1 infects astrocytes in the brain (Saito et al, Neurology ~1998) as well as T-cells in the blood, and the same types of HIV-1 infect both cell classes (Westervelt et al, ~1999). There is no means I am aware of by which to clear infected astrocytes, so the Esperanza patient, like the San Francisco, London and Berlin patients, must still harbor a brain residue of HIV-1 proviruses. However, in astrocytes HIV-1 does not express all its genes; rather, the NEF gene is overexpressed while the others are more or less silent. But biology is leaky, so the question is really what is it about elite resisters that prevents their astrocyte virus from accumulating enough full-length variants to ignite a new round of infection? Funding ran out before I could answer this question.