T cells are the other arm of the adaptive immune response (in addition to B cells) that are essential for clearing virus infections. Most studies of immunity to SARS-CoV-2 infection have focused on antibodies and their ability to neutralize virus infection. The observation that variants of concern are less effectively neutralized by antibodies against ancestral strains have led to predictions of vaccine failure and doom. This outlook is incorrect: amino acid changes in the spike protein of SARS-CoV-2 variants of concern do not impact T cell reactivity and are not likely to affect the ability of T cells to clear infection. This conclusion has been emphasized by the results of another study which show that SARS-CoV-2 variants of concern partially escape humoral but not T-cell responses in COVID-19 convalescent donors and vaccinees.
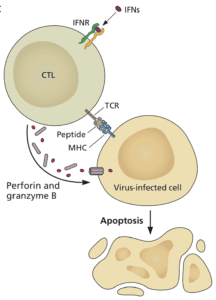
Cytotoxic T cells can sense that a cell is infected and kill it (illustrated). T cells sense infected cells by virtue of viral peptides that are presented by major histocompatibility molecules on the plasma membrane. Such T cell peptides may be produced from nearly any viral protein. In contrast, only certain viral proteins, like the spike of SARS-CoV-2, can give rise to antibodies that block infection. T cell epitopes are presented to T cells on the infected cell surface by MHC molecules, which are encoded by highly polymorphic genes. That means that your MHC is likely different from mine, and so will be the viral peptides displayed in them. So if a T cell epitope varies during your infection, it won’t matter to other people €“ their infected cells will be displaying different T cell peptides.
A study of antibody and T cell responses to SARS-CoV-2 and variants of concern B.1.1.7 and B.1.351 was carried out in a cohort of health care workers vaccinated with BNT162B2 mRNA vaccine. Some of these individuals had recovered from COVID-19 and received a single vaccine dose, while others had not been infected and received two vaccine doses.
Plaque assays were used to show that vaccine-induced antibodies neutralized the infectivity of B.1.1.7 virus as well as ancestral SARS-CoV-2. However, neutralization titers against the B.1.135 variant were about 4-fold lower.
To examine T cell responses to vaccination, blood mononuclear cells (PBMC) were stimulated with peptides from the spike protein. PBMC from immunized patients were activated equally by peptides spanning the entire spike protein from the ancestral virus, or from peptide pools covering the regions of spike that are changed in the variant viruses. As shown previously, T cell epitopes in the spike protein of variants of concern do not functionally change.
We can deduce the meaning of these findings for infection with variants of concern. In theory, should a variant fail to be efficiently neutralized by antibody in an individual previously infected with ancestral virus, or vaccinated (with ancestral spike protein), the T cells should still be able to prevent spread of infection and severe disease or death. This hypothesis is supported by the outcome of trials with the Johnson & Johnson Ad26.COV2-S vaccine, an adenovirus vectored spike vaccine. Sera from volunteers in South Africa, where B.1.351 circulates, had a tenfold reduced neutralization titer against that variant of concern. However, the vaccine was 100% effective in preventing hospitalization and death due to COVID-19 – likely a consequence of virus-specific cytotoxic T cells.
The situation with other vaccines is less clear. The AZD1222 vaccine, which showed 70% efficacy in the UK, showed only 22% efficacy in South Africa against mild to moderate COVID-19. Whether or not this vaccine would prevent severe COVID-19 could not be assessed as there was no serious disease observed during this trial.
The B.1.1.7 variant has the N501Y change in the spike protein, while B.1.351 and P.1 (Brazil) have in addition the amino acid changes K417N/T and E484K. Variant B.1.617 (India) has E484Q and L452R; the latter is also present in CAL variants. Given that none of these changes alter T cell reactivity it is likely that spike vaccines will protect against serious disease and death caused by these variants. Reports of reinfection with such variants in previously vaccinated individuals that leads to serious disease should be taken with a large grain of salt.

In the same (vaccines) way that prior infections protect us against future infections by means of cross-reacting T-cells, overcoming COVID-19 naturally offers great help to our own lives.
The question is, when will at least the minimum of T-cell activation become part of vaccine evaluations? We could have more virus proteins in our vaccines to improve coverage.
Hello,
So would you say that this is a ray of hope for organ transplant patients who in the John’s Hopkins study did not fare well at all in antibody protection?
Thank you!
I have chronic Cd8 Lymphocytopaenia – I have been vaccinated but should I expect this not to be as effective for me?
A recent study reported on a closer look at COVID-19 patients suffering from lymphopenia almost always exhibit significant decreases in T cell counts. Patients admitted to the ICU showed a drastic decrease in CD8+ T cells. on my view, I think the vaccine might work on you but there is that percentage of it not elicit the response fully hence fail to protect.
The Novavax vaccine is protein-only, and would not be expected to induce much of a killer T cell response. How significant a drawback is this for this vaccine?
Pingback: T cells will save us from COVID-19, part two - Virology Hub
In the city Manaus Bresil a significant proportion of the population caught Covid-19 during the first wave. At the end of 2020 the new variant P1 appeared. A lot of people who caught Covid-19 during the first wave caught it again with the P1 variant and they were sicker.
It seems that the immunity they built up after the first infection didn’t protect them from new variant.
The doctor Didier Raoult, a French physician and microbiologist specializing in infectious diseases said during an interview that the best immunity to Covid-19 is to have contracted the illness and healed. According to doctor Raoult previous infection is more effective than vaccination.