The blame for the return of poliomyelitis is the drop in immunization rates to 66%. Coverage of at least 95% of the population is needed to prevent outbreaks of the disease. There are likely several reasons for the drop in coverage, including erosion of public confidence in vaccines caused by problems with Dengvaxia, the dengue vaccine, and reductions in the nation€™s health budget.
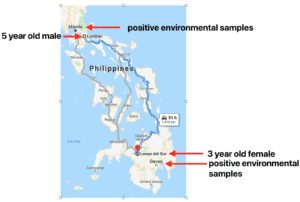
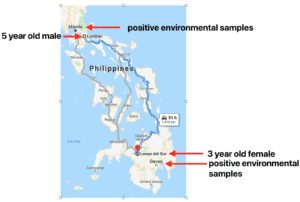
The two cases of poliomyelitis were in a 5 year old male in the north and a 3 year old female in the south (illustrated). Poliovirus-positive environmental samples were also found near both locations. These observations indicate that polioviruses are likely circulating throughout the country.
The two cases of poliomyelitis were caused by vaccine-derived poliovirus type 2. The main vaccine used for the poliovirus eradication effort is an infectious, attenuated preparation called oral poliovirus vaccine (OPV), developed by Albert Sabin. During replication in the intestine, it confers immunity to infection and also changes genetically and re-acquires the ability to cause paralysis. These vaccine-derived polioviruses can circulate in the population and cause outbreaks of poliomyelitis.
The last case of paralysis caused by wild (e.g. non-vaccine) poliovirus type 2 occurred in 1999 in India. However, type 2 circulating vaccine-derived polioviruses (cVDPV) continued to cause outbreaks of poliomyelitis. Consequently it was decided, in 2016, to stop immunizing with type 2 OPV. Currently bivalent OPV is used which contains only poliovirus serotypes 1 and 3. Because vaccine-derived poliovirus type 2 continues to circulate, WHO has recommended that a dose of trivalent inactivated polio vaccine (IPV) also be given to reduce the likelihood of infection with this serotype.
The childhood vaccine schedule in the Philippines includes both IPV and bivalent OPV. Hence the recent outbreak can be explained by a drop in immunization rates. Other outbreaks of vaccine-derived type 2 have occurred in recent years in areas where immunization coverage drops, such as in Syria in 2017.
The response to the Philippine polio cases will be mass administration of monovalent OPV2, which is more effective than IPV at halting outbreaks. Unfortunately this immunization will also re-introduce vaccine-derived polioviruses into the population.
Outbreaks of vaccine-derived poliovirus are likely to continue as long as OPV is used and vaccine coverage drops in specific areas. A solution would be to immunize globally only with IPV. However such a strategy is problematic due to the need to inject this vaccine and manufacturing shortages. Meanwhile high rates of immunization are essential to protect children from paralytic disease.

Pingback: Sociedad Española de VirologÃa | SEV
Pingback: TWiV 567: Outbreaks and a breakout | This Week in Virology