…it has been proposed that soluble cell receptors might be effective antiviral therapeutics. It has been suggested that mutants resistant to the antiviral effects of soluble receptors would not arise, because mutations that abrogate binding to receptors would be lethal.
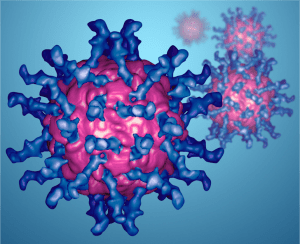
We had previously shown that the cell receptor for poliovirus, CD155, produced in a soluble form, would bind to poliovirus (pictured – the very image from the banner of this blog), blocking viral infection. We then found that it was relatively easy to select for soluble receptor resistant (srr) virus mutants. These viruses still enter cells by binding to CD155, but the affinity of virus for the receptor is reduced. Poliovirus srr mutants replicate normally in cell cultures, and cause paralysis in a mouse model for poliomyelitis. We speculated that receptor binding might not be a rate-limiting step in viral infection, and short of abolishing binding, the virus can tolerate a wide range of binding capabilities.
The amino acid changes that cause the srr phenotype map to both the exterior and the interior of the viral capsid. The changes on the virion surface are likely to directly interact with the cell receptor. Changes in the interior of the virus particle may be involved in receptor-mediated conformational transitions that are believed to be essential steps in viral entry.
When this work was done, clinical trials of soluble CD4 for HIV-1 infection were under way. We believed that our findings did not support the use of soluble receptors as antivirals, which we clearly stated in the last sentence of the paper:
These findings temper the use of soluble receptors as antiviral compounds.
HIV-1 mutants resistant to neutralization with soluble CD4 were subsequently isolated, and the compound was never approved to treat HIV-1 infection in humans for this and other reasons, including low affinity for the viral glycoprotein, enhancement of infection, and problems associated with using a protein as a therapeutic.
Recently a new soluble CD4 was produced which also includes the viral binding site for a second cell receptor, CCR5. This molecule overcomes many of the issues inherent in the original soluble CD4. It provides broad protection against a wide range of HIV-1 strains, and when delivered via an adenovirus-associated virus vector, protects nonhuman primates from infection. This delivery method circumvents the issues inherent in using a protein as an antiviral drug. Because this protein blocks both receptor binding sites on the viral envelope glycoprotein, it might be more difficult for viruses to emerge that are resistant to neutralization. The authors speculate that such mutants might not be efficiently transmitted among hosts due to defects in cell entry. Given the promising results with this antiviral compound, experiments to test this speculation are certainly welcome.
