In the introduction to their paper, published in the Journal of Virology, the authors note other problems with many of the studies of XMRV in CFS patients:
- Too small control populations
- Patient and control samples collected at different times
- Investigators generally not blinded to sample identity
- PCR assays that rely on conservation of viral sequence mainly used
- Limits of detection, reproducibility, and precision of assays unknown
- Controls for each step that would identify analysis not done
- Insufficient numbers of negative controls included
- No study included positive samples from the original 2009 patient cohort of Lombardi et al.
To address these issues, the authors collected blood from 105 CFS patients and 200 healthy volunteers in the Salt Lake City area. One hundred of the patients fulfilled both the CDC-Fukuda and the Canadian consensus criteria for diagnosis of ME/CFS. The patients were selected from a clinic that specializes in the diagnosis and management of CFS and fibromyalgia.
New blood samples were also collected (by a third party) from 14 patients from the original study by Lombardi et al. The samples were blinded for subsequent study. Detection of viral nucleic acids was done using four different PCR assays. Anti-XMRV antibodies in patient sera were detected by ELISA. Finally, virus growth from clinical specimens was attempted in cell culture. The authors used the multiple experimental approaches reported by Lombardi and colleagues.
Let’s go through the results of each assay separately.
PCR for viral nucleic acids. Four different quantitative PCR assays were developed that detect different regions of the viral genome. The assay for pol sequences has been used by several groups and is the most specific PCR assay for XMRV. Three other PCR assays were also used that target the LTR, gag and env regions of XMRV DNA. These assays could detect at least 5 viral copies of XMRV DNA. The precision and reproducibility of the PCR assays, as well as their specificity for XMRV, were also demonstrated. DNA prepared from white blood cells of 100 CFS patients and 200 controls were negative for XMRV. For every 96 PCR reactions, 12 water controls were included; these were always negative for XMRV DNA.
XMRV antibodies in human sera. To detect XMRV antibodies in human serum, a portion of the viral envelope protein, called SU, was expressed in cells and purified from the cell culture medium. The SU protein was attached to plastic supports, and human serum was added. Any anti-XMRV antibodies in human sera will attach to the SU protein and can subsequently be detected by a colorimetric assay (we have discussed this type of assay previously). This assay revealed no differences in the amount of bound human antibodies for sera from CFS patients or healthy controls. Some of the patient sera were also used in western blot analysis. Recombinant XMRV SU protein was fractionated by gel electrophoresis. The protein on the gel is then transferred to a membrane which is mixed with human serum. If there are anti-XMRV antibodies in the human serum, they will react with the SU protein on the membrane, and can be detected by a colorimetric assay. When rabbit anti-XMRV serum was used in this assay, the SU protein was readily detected. None of the human sera analyzed by this method were found to contain antibodies that detect SU protein.
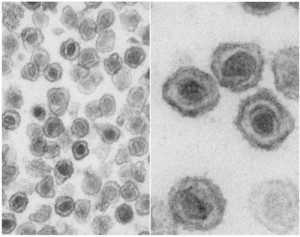
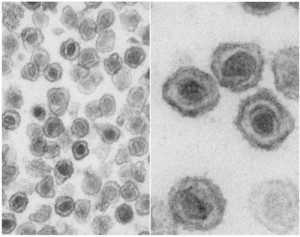
Infectious XMRV in human plasma. It has been suggested that the most sensitive method for detecting XMRV in patients is to inoculate cultured cells with clinical material and look for evidence of XMRV replication. The XMRV-susceptible cell line LNCaP was therefore infected with 0.1 ml of plasma from 31 patients and 34 healthy volunteers; negative and positive controls were also included. Viral replication was measured by western blot analysis and quantitative PCR. No viral protein or DNA was detected in any culture after incubation for up to 6 weeks.
Analysis of previously XMRV-positive samples. Blood was drawn from twenty-five patients who had tested positive for XMRV as reported by Lombardi et al. These samples were all found to be negative for XMRV DNA and antibodies by the PCR and ELISA assays described above. In addition, no infectious XMRV could be cultured from these 25 samples.
Presence of mouse DNA. After not finding XMRV using qPCR, serological, and viral culture assays, the authors used the nested PCR assay described by Lo et al. Although positives were observed, they were not consistent between different assays. This led the authors to look for contamination in their PCR reagents. After examination of each component, they found that two different versions of Taq polymerase, the enzyme used in PCR assays, contained trace amounts of mouse DNA.
Given the care with which these numerous assays were developed and conducted, it is possible to conclude with great certainty that the patient samples examined in this study do not contain XMRV DNA or antibodies to the virus. It’s not clear why the 14 patients resampled from the original Lombardi et al. study were negative for XMRV in this new study. The authors suggest one possibility: presence of “trace amounts of mouse DNA in the Taq polymerase enzymes used in these previous studies”. I believe that it is important to determine the source of XMRV in samples that have been previously tested positive for viral nucleic acid or antibodies. Without this information, questions about the involvement of XMRV in CFS will continue to linger in the minds of many non-scientists.
At the end of the manuscript the authors state their conclusion from this study:
Given the lack of evidence for XMRV or XMRV-like viruses in our cohort of CFS patients, as well as the lack of these viruses in a set of patients previously tested positive, we feel that that XMRV is not associated with CFS. We are forced to conclude that prescribing antiretroviral agents to CFS patients is insufficiently justified and potentially dangerous.
They also note that there is “still a wealth of prior data to encourage further research into the involvement of other infectious agents in CFS, and these efforts must continue.”
Clifford H. Shin, Lucinda Bateman, Robert Schlaberg, Ashley M. Bunker, Christopher J. Leonard, Ronald W. Hughen, Alan R. Light, Kathleen C. Light, & Ila R. Singh1* (2011). Absence of XMRV and other MLV-related viruses in patients with Chronic Fatigue Syndrome. Journal of Virology : 10.1128/JVI.00693-11

You struggle with every little bit. Evidence is in the data, the observations.
Yet, when the CDC rested 20 they were negative for contamination.
The assays were validated by the other methods in Lombardi et al and through Lo et al. XMRV is a hybrid of a poly and xeno.
Validation is an important and necessary step in the creation of any assay.
Serology was performed by the CDC and NCI. The WPI results outside the study matched those of the NCI. 2 of the 5 people in total were positive for both day 0 and day 2. 2 others on different days. The waxing and waning of the disease may account for these differences. The conclusion was that the study was too small and further research was needed.
Is this published somewhere? If not, then the data can’t be used according to your own standards.
You again did not answer the question? Who are the regulators, and why do you keep stating this?
RRM, I am too keen on these techniques of redirecting discussion and deflecting arguments. Let’s return to my original and only question. I will repeat it in its most basic form:
There are two unknowns in this study:
1) Did any of the clinical samples contain XMRV?
2) Could the methods in this paper detect XMRV in these clinical samples conditional on it being present?
The authors *clearly* concluded that the answer to #1 is definitively “no.” I claim they never ruled out #2 and therefore drawing any conclusion about either question is illogical and unscientific.
Now, my question: How did the authors demonstrate conclusively that the answer to #2 is “yes” (thereby justifying their conclusion)? If they did not do this, how can you justify their conclusion as anything but utterly unfounded?
This question pertains *entirely* to the details of this paper alone. It does not concern the WPI’s study and your fixation on how they “validated” their own samples. Nor are your various fallacious appeals to history, authority (“scientific philosophers”), and credentials/reputation (a paper, not a blog!) relevant to this question.
It is a simple, straightforward question of evidence and logic.
*blink*
I’m sure this will bring on even more vitriol, and I will not engage further, but this may be one of the reasons why most people eventually shrug and walk away. I fail to see the point of being so antagonistic that no one wants to engage with patients or study CFS.
ME/CFS appears to be a intellectually fascinating and complex field, and there is very little doubt that more biomedical attention is warranted, but there are other fields offering much more prestige and money and you don’t have to put up with being insulted by desperate people. And that is a shame, but it appears to be in part a situation of patients own making if this thread is any indication.
I am aware that patients struggle with cognitive dissonance, but what has really been accomplished by taking offense at the most neutral and innocuous of statements and twisting the meaning to the point where it is nonsensical? This is a science blog not a conspiracy blog. There are probably more appropriate forums for many of the statements on here.
ciao
Pingback: Ian Lipkin on XMRV
realistically there are THOUSANDS of retroviruses out there… all sorts of them… tons of pathogens
we just have to spend more money researching pathogens, and eventually it will be found 🙂
I trust Ila Singh. I don’t know why people have to denigrate the results.
I advocated very early on that the research had to move forward, and now that it has I am happy they finally got to the bottom of it.
I would like to point out that the problems many people are noting with the posts on here (i.e. scientists being “on our side” when they agree and on “the other side” ) has happened because people had to believe in a person instead of an institution. Science replaced religion (historically) because it gives a reason for things that are unexplained. What you are witnessing, are not people that believe in a figure (or an institution) because they want to… but because they need to. Its bordering on religious conviction at times, and that is sad because of what it shows is lacking in the response they have received to their illness. These are people that feel they have been failed by traditional institutions. You gotta give the people something to hold on to. Give the people hope.
rrm…time 4 u to read what lipkin thinks abt singhs’s study…..her study just added more confusion to a an already confused pic….not very high praise for a study you are so stoughtly defending.
Who is “you” in your post? Prof Racaniello? I don’t think Prof Racaniello has to be single-handedly responsible for campaigning against every single occurrence of unnecessary medication use etc. We wouldn’t expect him to be responsible for climate change and democracy in the middle east as well would we?! I think he goes well beyond the call of duty as it is.
@e9356e538e7454b10550f923e2b052e4:disqus kellylatta: I would be sorry to see you go, and even sorrier to hear that you have decided to tar all “patients” with the same brush of being “vitriolic” and “insulting.”
Would you interpret my words differently if you knew they came from a professional writer and editor with a lifetime’s experience in using language, who has also taught writing and heard reactions such as yours directed toward “the mean picky teacher” rather than the “crazy vitriolic patient?” I’ve even taught science writing, a little; a specialty where I think you could argue that clarity of meaning has even higher stakes than in other fields. We’ve all seen the distortions in public understanding of science, and how much those distortions are aided and abetted by the dismal standard of science journalism as well as the failure of public agencies to communicate appropriately with the public. (Seth Mnookin has had some very to-the-point comments to make about this, with regard to the anti-vaccine hysteria.)
The first response I wrote to you was an appreciation for your attempt to answer a patients’ question in a thoughtful and respectful way, and I still mean that. If I follow up with another response in which I say I have trouble understanding a point you’re making because of the words you’ve chosen, and go on to further express my opinion that some of the language you’re using isn’t the right instrument for the kind of point you seem to want to make, would you read that criticism differently if it came from a colleague, maybe even a senior colleague, instead of someone whose credibility is immediately suspect because she is a “patient” first and foremost?
Well, it’s a terrible thing to have happen to one’s career as well as to the credibility of all one’s statements; I hope you never have to experience it yourself. (Have you noticed that, in many of the books written by doctors who themselves become gravely ill and forced into the “patient role,” a common theme is usually horror at how an intelligent, professionally accomplished, knowledgeable person suddenly becomes disempowered and even infantilized by their colleagues’ attitudes?)
You seem like a caring and knowledgeable person; whatever your role actually is in science and medicine, I hope you go on to continue to sharpen your tools and use them wisely.
Ila Singh’s group did use the same methods. You wouldn’t expect doubling the Platinum Taq and using dUTP instead of dTTP to change the results substantially. There are many diagnostic PCR assays out there with equal or greater variation than this and they don’t make this degree of difference. You would expect the nucleic acid extraction step to have a much greater effect and this paper, Lombardi et al and Lo et al all used Qiagen kits.
“Now, my question: How did the authors demonstrate conclusively that the answer to #2 is “yes” (thereby justifying their conclusion)?”
You keep spinning in circles. The whole point of the argument is: how could the authors ever demonstrate conclusively that the answer is “yes” if there is no XMRV present in clinical samples? Because you cannot anwer that, your whole line of argument is useless.
And note that by using your logic, the WPI study is just as flawed, as there were two unknowns in that study also:
1) Did any of the clinical samples contain XMRV?2) Could the methods in that paper detect XMRV in clinical samples?
..Etcetera, etcetra…
Finally, I am not making fallacious appeals to history. If you would read the comments, you would see that several poster assert or imply that this is the normal way in which science makes progress. Demanding a historical example is then a very normal reply to that (wrong) assertion. The fact that nobody can give me such an example, indicates that this methodology is new and unprecedented.
Now, that doesn’t mean it is worthless by definition, but it has to make one think. The best way for new scientific methodology to get accepted, is not by presenting it at blogs, but to present it to peers (as many scientific philosophers have done before you. You are implying that the peer review system is a fallacious appeal to authority). Until this new and unprecented methodology is accepted by the scientific community instead of on a single patient forum, it’s really not very useful in this discussion.
I struggle with every bit? You even struggle with a simple definition of “evidence”.
I simply look at the available data and publications. The original study by Mikovits mentioned XMRV and CFS. The Lo-Alter study mentioned MLV and CFS. The Oxford criteria are for CFS, so are the Fukuda criteria. The Canadian Consensus Criteria are for ME/CFS. Where is the ME in all of this?
I am very well aware of the differences between the criteria, and ME vs CF according to the WHO. But if you want to stick to the science, the recent biomedical research doesn’t mention ME, but CFS. Show me a publication on XMRV and ME. Show me a publication on HGRV. And with publication I don’t mean a patient’s blog, but a scientific publication in a journal.
@a2dc987c71224598a61d1888e27a0720:disqus What I meant to say was I’m not really interested in medicine or science, except for the fact that they impact on the disease I have. The fact that medicine and science don’t really interest me doesn’t change the fact that I’ve studied this for years and so have formed conclusions based on the facts and the science. We absolutely have been consistently abused by the UK and US governments. The mountain of evidence shows this. Much of it is in Osler’s Web. I suggest you read it. It is very readable as well as exhaustively informative.
For one example of the intentional warping of the science, just look at the Sharpe 1991 CFS definition which defines Idiopathic CF, not ME (“CFS”). The UK psychiatrists just then keep publishing and publishing on this patently invalid definition (in addition to claiming that it is psychogenic based on no evidence). Pls also see urbantravels excellent post earlier on the subject of ‘conspiracy’. Here’s an excellent vid; a trailer for the upcoming documentary “What about ME?”:
http://vimeo.com/10536172
I don’t know if HGRVs are associated with ME or not. I don’t think the science has been sorted out 100% yet so I think Singh’s saying that “XMRV is not associated with CFS” is premature. I think the study she did was very good (but once again I am a layperson so can’t totally evaluate it). I have not yet been tested for XMRV because I would like to wait for clearer answers from the Science. It’s possible WPI, NCI, Cleveland Clinic, NIH and FDA are wrong. It’s also possible XMRV is associated with ME but not significantly pathogenic. I don’t think we know yet.
I’m not referring to the statement by Prof. Klimas that she’d rather have ME than HIV. I’m referring to Infectious Disease Prof. Mark Loveless’ early 1990’s testimony to Congress that his ME patients’ Karnofsky morbidity scale scores were equivalent to those of his AIDS patients in their last weeks of life. And to Dr. Dan Peterson’s finding that his patients’ MS-36 physical functioning scores were, with the apparent exception of a few cancers, the lowest of any disease yet measured.
(Osler’s Web p.364 http://www.amazon.com/Oslers-Web-Labyrinth-Syndrome-Epidemic/dp/0595348742/ref=sr_1_1?ie=UTF8&s=books&qid=1304757370&sr=8-1 )
I say “untreated AIDS” because the treatment for AIDS at that time, I believe 1991, was close to what we would consider ‘untreated’ today. Certainly the treatment didn’t work very well since he was referring to AIDS patients just about to die.
“Singh bent over backward to try to use the same assays as published,
allowing her to knock down what I consider to be a real straw man but
that
nonetheless was out there,” says retrovirologist John Coffin of Tufts
University in Medford, Massachusetts. Coffin initially supported theScience report but subsequently concluded, with many others, that XMRV is a contaminant. In a recent study he provided evidence that the virus accidentally originated during mouse lab experiments.
Singh says she and her co-workers also had problems with
contamination. When they ran one PCR assay that had been used in the
original Science
Science paper,
retrovirologist Judy Mikovits of the Whittemore Peterson Institute for
Neuro-Immune Disease in
Reno, Nevada, isn’t persuaded by the Singh group’s inability to
detect XMRV in anyone. “I was astounded when I leaned that Ila [Singh]
didn’t find it,”
says Mikovits. “These are good scientists.” Science paper. We don’t think any of it
is wrong. There is no evidence of contamination in our lab, and we have controlled for that all along.” Singh counters that although some protocol differences exist, they
worked closely
with Mikovits’ team to replicate the original work. Singh says
the fact that they didn’t find XMRV in any of these patients is
significant. “She
[Mikovits] pointed us toward patients that she had repeatedly
tested positive,” says Singh. “We should have found at least one that
was positive. Not
all of them would have gone negative on the day when a
phlebotomist met with them.”Science report did not assert
that XMRV causes CFS but only claimed to have detected XMRV in CFS
patients. But the
large community of CFS patients, who often find themselves
confronting a medical establishment that questions the very existence of
their disease,
pounced on this finding, and some even started taking
antiretroviral medicine to treat their supposed XMRV infections. http://news.sciencemag.org/scienceinsider/2011/05/more-bad-news-for-chronic-fatigue.html?ref=hp
Why does he say in the paper’s title that PC is not associated with XMRV if he found it in 2% of pwPC? (this isn’t sarcastic; I am curious)
Ooops that didn’t come out very well sorry. Here’s an interesting bit from the article:
‘Singh says she and her co-workers also had problems with contamination.
When they ran one PCR assay that had been used in the original
Science
http://news.sciencemag.org/scienceinsider/2011/05/more-bad-news-for-chronic-fatigue.html?ref=hp
Further quotes from those involved are coming out in your papers now I see. Here’s a link to a Tsouderos article. Am interested in the additional information these carry, and not the journalistic opinion:
http://www.baltimoresun.com/health/boostershots/la-heb-xmrv-chronic-fatigue-20110506,0,3774692.story
Again you make statements based on assumptions that are not proven true, yet you treat them as givens. There is no such thing as a “population level” of XMRV in the blood, that is not a given. The findings in PC are in tissue, not blood. How the latest studies impact XMRV/PC I honestly do not know, ie is that still considered valid. You then criticize Singh for using a novel blood assay for this study. Didn’t Lombardi et al also use a novel blood assay, according to Gob adapted from some other methodology? Using you own arguments, the Lombardi study is similarly “unvalidated” because it used a novel assay and was not calibrated against known clinical positives. That is the crux of the whole point here, you are being completely inconsistent, almost arbitrary in what you consider valid or invalid, based purely on whether you like the results or not. That is not scientific. You keep claiming the Singh studies were not a true replication study. A number of scientists, who know far more about the design or these studies and the assays involved than you or I do, consider it comprehensive and as close to complete replication as possible. So far, the only scientist I’ve seen criticize the study at all is Mikovits herself, and her comments were vague, so what does that tell you?
@a2dc987c71224598a61d1888e27a0720:disqus How am I doing “untold damage to the reputation of CFS patients in the research world”? If it is because I am saying that I’m upset because we have been subject to the CDC, NIH, UK govts and band of UK psychiatrists’ 27 year war on ME science and patients, then so be it. I’m not going to go the back 0f the bus any more and if ‘the research world’ doesn’t like that sentiment then it can go to hell. I am sick and tired of having to patrol the ‘scientists’ like a hawk. I’d like to devote my energy to healing not making sure we are being persecuted.
Nobody here can even mention one replication study in the field of (retro)virology that was a closer replication of the study it was trying to validate than the Singh study.
What does this tell us?
a) The definition of “replication study” used is wrong
b) There has never been a replication study in the history of retrovirology
c) Retrovirology is actually not science
Nobody has “got to the bottom of it” yet. I am rather perturbed at the number of times various people are writing-off XMRV as being in association with ME/CFS, when none of the experimental data suggests such a positive conclusion. The titles of the articles go beyond the deductions possible from the experiments. To me, this is a bit sinister, as in “methinks the lady doth protest too much”.
Seriously, setting aside any “conspiracy” theories, why has there been such a spate of negative papers and comments, including all the stuff on contamination, none of which detracts from the original paper’s findings? The contamination theory is just that – there is no proof that Lombardi et al’s XMRV was the result of any contamination. The same applies to the potential generation of the novel virus within the laboratory, while the disease has been around a minimum of 100 years.
@578f6c5c347c88a5d61a1a25b2700dd9:disqus
“Do you think there’s sufficient evidence to warrant further research regarding infectious agents & CFS?”
Even Greg Towers admits there’s sufficient evidence. Next!
So you seem to concede that you cannot answer this question. Therefore neither you nor the authors of this paper can justify their conclusion that none of the samples contained XMRV. This is simple logic. A clear, parsimonious, alternative explanation was not ruled out.
Everything else you’re going on about here is, ironically, your problem not mine. The burden of proof is on *you* to prove that the results are logically sound if you want to argue that they are. But, alas, you cannot and this study remains fundamentally flawed.
I agree that it is not easy to rule out #2 as the explanation for the findings, but it was not ruled out nor is it my burden to do so.
Pingback: Contagions Round-up 8 « Contagions
It is you who conceeds that he is unable to answer my simple bus essential question.
Since you don’t accept my explanations, accept another example:
– Researcher A: I have detected the monster of Loch Ness using my methodology
– Researchers B-Z: we cannot detect it
– Researcher A: You have two variables in your experiments: 1) Does the lake contain the Loch Ness monster and 2) Is my methodology capable of detecting Loch Ness monsters. Therefore I am right and you are wrong and I won’t answer your basic and simple questiosn that would simply prove you wrong [puts fingers in ears] lalalala….
Please explain what is wrong with the above example without shooting your own “methodology” in the foot. Oh, I know, your logic is watertight, so you don’t have to… 😉
You must also notice that he has not a single word of factual criticism for Singh’s study or her methodology. He does not criticize the methodology, but knows that the results will not settle the public debate, as only a blinded retest by the original lab(s) involved can settle the issuse. That is exactly why he is the leader and independent arbiter of such a study.
I predict that, when the Lipkin study will find nothing, all the pro-XMRV people will just see all the pieces of the conspiracy coming together. All other negative studies led the patients in the hands of the “independent” Lipkin, which of course was the set-up to convince everybody that XMRV is not real (in CFS).
How are you looking in the lake? That would be part of the methodology. Science is in the variables, not only the parts you don’t leave out.
Pingback: XMRV/ME/CVS en Human “Rumor†Virussen VI « Cryptocheilus Weblog
What is there to criticise in any study. It is very clear that none have replicated the Lombardi or Lo methodology. Thus the results cannot effect each other. We all learn nothing. But if you wish to say they do impact on the results of another study, then criticism is appropriate as they were not designed to test the original findings.
Yes it is.
How can you not know who the regulators are?
Thank you for proving my point.
Shin et al
“We could reliably detect less than 5 copies of XMRV plasmid DNA in a background of 400 ng of human placental DNA”
Plasmid, not a clinical sample.
You are very welcome.
[Still waiting for a definition of evidence, an example of a true replication study or an example of an independent validation study that calibrated its assays to the supposed positives of the study is was trying to validate, from you or any other top scientist from the mecfsforums]
I use a very special and ultra-sensitive and home developed nested RT-PCR assay to check the lake’s water for DNA of the monster.
And there is no way you can prove me wrong!
You do know that, in this context, Roy means “published in a peer reviewed journal”? Even though I believe the assertion to be true, we just don’t know the conditions of said experiment (as it is unpublished).
And Gob, you do know that testing for contamination would only detect MOUSE DNA? Therefore, if (for instance) those samples were contaminated with XMRV that originated from HUMAN cell lines (which, I might add, is not unlikely), they would have been negative for mouse DNA contamination.
Unless I replicate your methodology exactly and produce a different result.
It is published.
There is no evidence that the positive results were caused by contamination from a cell line, or that a cell line is the source of contamination. The same goes for the other variants of HGRV. You would also not have an immune response to an MLV virus from a contaminant.
Shin et al was not a replication study.
Have you still not found one amongst all those available?
Have you not found one example in all those available?
You have then proved that you didn’t actually replicated my exact methodology as, if you would, you would have gotten the same results as me.
And I promise you that you would get the same result as me if you would calibrate your assay to my “known positive”.
I was just giving an example of contamination which testing for mouse contamination would not detect. You said above that the samples were negative for contamination, while the samples were negative for *mouse* contamination.
By your own (illogical) reasoning, Mikovits was pretty dumb to check for mouse contamination, as there was also no evidence for it. Then why check for mouse contamination?
Just like mouse contamination has to be considered even when there is no evidence for it (that is why you check), human cell line contamination has also to be considered.
(Oh, it’s not published)