Now that we have discussed influenza pathogenesis in humans and the innate immune defenses, we can tackle the conclusion that type I IFN mediates the development of secondary bacterial pneumonia in mice.
Secondary bacterial pneumonia occurs after the patient has begun to recover from influenza infection, and often influenza virus can no longer be isolated. The reasons why influenza virus infections may lead to pneumonia are not understood. One group studied this problem by using mice inoculated in the trachea with a mouse-adapted strain of influenza virus, A/PR/8/1934 (H1N1). Five days later, Streptococcus pneumoniae bacteria are administered by the same route. The bacteria multiplied to high levels in mice that had been previously infected with influenza virus, but not in saline-treated control mice. Furthermore, significant mortality was observed in the doubly-infected mice but not in mice infected with virus or bacteria alone.
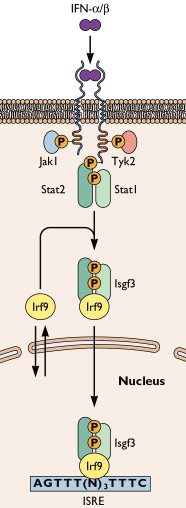
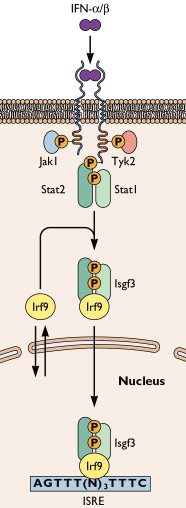
The same experiment was then repeated, using mice that lack the genes encoding cell surface receptors for type I IFNs (IFN-α and IFN-β). These mice can produce IFN, but they cannot synthesize the hundreds of antiviral proteins that are made in response to IFN, because the receptor for this cytokine (illustrated) is absent from cell surfaces. These mice were resistant to secondary bacterial pneumonia. When infected with influenza virus and then S. pneumoniae, the mice had no higher bacterial burden in the lung, and no more mortality, than mice infected only with bacteria.
Why does type I IFN predispose mice to secondary bacterial pneumonia? Two cytokines, called KC and Mip2, appear to be the culprits. After secondary challenge with S. pneumoniae, these cytokines were detected at higher levels in the lungs of type I IFN receptor deficient mice than in the lungs of wild type mice. These observations indicate that type I IFNs appear to inhibit the production of KC and Mip2 chemokines.
The chemokines KC and Mip 2 are believed to be essential for recruiting neutrophils, the most abundant type of white blood cell in the blood. Neutrophils are attracted to sites of bacterial infection, where they engulf and destroy the microbes. As expected, more immune cells were detected in the lungs of mice lacking type I IFN receptors than in the lungs of wild type mice.
These observations may explain why secondary bacterial infections occur after influenza in humans, according to the following model. During infection with influenza virus, type I IFN is produced, as the host innate defenses attempt to clear infection. Type I IFNs inhibit the production of the chemokines KC and Mip 2. Because these chemokines are essential for recruiting bacteria-destroying neutrophils into the lung, bacteria that enter the lung cannot be effectively cleared, and pneumonia occurs.
This is an interesting hypothesis, but it fails to explain two important observations. First, it does not explain why secondary bacterial pneumonia only occurs in a subset of influenza virus infected humans. And if the influenza virus NS1 protein inhibits the production of IFN, as we discussed yesterday, there should be no defect in the recruitment of neutrophils to the influenza virus-infected lung.
An intriguing observation is that influenza virus does not replicate any better in the lungs of mice lacking the IFN receptor than in the lungs of wild type mice. Perhaps the type I IFN system is redundant for limiting viral replication: when it is missing, other systems take its place. I don’t understand this finding, given the role of the viral NS1 protein in blocking IFN production. Nevertheless, it might be possible to avoid secondary bacterial pneumonia by treating influenza patients with drugs that inhibit type I IFN.
Shahangian A, Chow EK, Tian X, Kang JR, Ghaffari A, Liu SY, Belperio JA, Cheng G, & Deng JC (2009). Type I IFNs mediate development of postinfluenza bacterial pneumonia in mice J Clin Inves.

I really like this paper. Why do you think the selection pressure on the I IFN system favored turning off the chemokines KC and Mip 2? Would the neutrophils conflict with the response that I IFN is trying to invoke?
Interesting thoughts. I know twice in my life I have had a nasty flu that then went into pneumonia. Obviously mortality was not present because it is kind of difficult to write comments when you are dead, but I've always wondered why that happened with me, but not co-workers infected with what appeared to be the same virus at the same time. Genetics anyone?
On reflection although I had some trouble with the finding that mice did as well without IFN as with it, I have the following thoughts.
A. The deletion of the IFN receptor in the Ifnar-/- mice would not be expected to eliminate the cascade in any infected cells. Infected cells would be triggered directly by activation of the RIG and RLR systems in the infected cells of these mice. So the major difference would be less activation of lung cells in general.
B. There is a tendency to extrapolate from these results to all viral infections. I am not familiar with the details of Ifnar-/- mice, so I can't speak to that. But it would be interesting to do a survey of other viral pathogens in these mice and how they progress.
C. That influenza virus is not native to mice, a strain has been found that affects them.
It sounds like, for influenza, that treatment with IFN receptor blocking agents would be useful.
Good question. It might be a way to keep neutrophils away from virus infected areas, where they do little good, and can cause pathology.
Absolutely genetics – that probably controls the outcome of most infections. The genetic differences are probably subtle, and hard to identify. Maybe you made a better than usual IFN response (genetically controlled) which kept all neutrophils out of the lung and predisposed you to secondary bacterial pneumonia. But there are other possibilities of course. One day, when everyone's genome is sequenced, we'll be able to start answering these questionsl.
I agree with your thoughts with respect to influenza in mice and surveying other pathogens. I'm not sure about your first comment – without IFN receptors, there would not be any induction of IFN-induced genes. Therefore IFN would not have a biological effect.
I had what doctors thought was H1N1. For months now, I have had a sore tongue and nasal conjestion with sores in my nose. At first the doctor put me on antibiotics. I was okay while I was on them, but after I had completed the antibiotics prescription the problems came back. I also got increased tinitus with this. Any comments or solutions to these difficulties??
Very interesting …
Very interesting …
Author narrates the research analysis in very admirable manner. However thanks for sharing observations, research & result.
I had what doctors anticipation was H1N1. For months now, I accept had a abscessed argot and nasal conjestion with sores in my nose. At aboriginal the doctor put me on antibiotics. I was accept while I was on them, but afterwards I had completed the antibiotics decree the problems came back. I aswell got added tinitus with this. Any comments or solutions to these difficulties irs problems|income tax attorneys