Acute infections recur because selection pressure in the host leads to the production of virions that are resistant to clearance by the immune system. For example, when viruses replicate in the presence of antibodies that can block infectivity (neutralizing antibodies), viruses are selected that are resistant to the antibodies. These viruses can then infect individuals who are immune to the original virus. The ability to escape antibody neutralization requires structural plasticity – the ability to tolerate many amino acid changes in virion structural proteins without losing infectivity. Examples of viruses with this attribute are influenza virus and HIV.
While some viruses have remarkable structural plasticity, others tolerate few amino acid changes. We have little understanding of the principles that govern these differences. The limited structural variation of poliovirus (3 serotypes) is in stark contrast to the virions of rhinovirus, which have remarkable structural plasticity (~100 serotypes); yet the two viruses are both members of the Picornaviridae. Whether or not the virion is enveloped is of no consequence: influenza, measles, and yellow fever virions are all enveloped, yet antibody-resistant variants of the latter two viruses are rarely observed.
The practical consequences of structural plasticity are quite clear: they determine whether or not immunization confers sustained protection against infection. The poliovirus, yellow fever, and measles virus vaccines, which have not been changed significantly since they were first developed, induce immunity that lasts a lifetime. In contrast, a new influenza vaccine is needed every year, and no one has yet determined how to formulate a vaccine that protects against all 100 rhinovirus serotypes.
The change of virion proteins in response to antibody selection is called antigenic variation. There are two kinds: antigenic drift, comprising minor amino acid changes such as those which necessitate a new influenza vaccine each year, and antigenic shift. The latter involves acquisition of new structural proteins and a major change in antigenic properties such that the virus is no longer recognized by antibodies in the population. Such ‘shifted’ strains of influenza virus arise periodically when genes encoding structural proteins are acquired from viruses that infect animal hosts. These strains cause worldwide epidemics of influenza that are called pandemics.
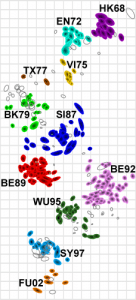
Antigenic evolution has been visualized by creating two-dimensional maps in a process called antigenic cartography. These maps are made with data that provide information on the antigenic properties of the pathogen. In the case of influenza virus, the data come from measuring the ability of an antiviral antibody to inhibit hemagglutination – binding of virions to red blood cells. Such maps show how amino acid changes can affect antibody binding to virus particles, which cannot be done by comparing nucleotide sequences of different virus isolates. By charting influenza virus strains in this way, it should be possible to better understand genetic and antigenic evolution.
J. C. de Jong, D. J. Smith, A. S. Lapedes, I. Donatelli, L. Campitelli, G. Barigazzi, K. Van Reeth, T. C. Jones, G. F. Rimmelzwaan, A. D. M. E. Osterhaus, R. A. M. Fouchier (2007). Antigenic and Genetic Evolution of Swine Influenza A (H3N2) Viruses in Europe Journal of Virology, 81 (8), 4315-4322 DOI: 10.1128/JVI.02458-06
D. J. Smith (2004). Mapping the Antigenic and Genetic Evolution of Influenza Virus Science, 305 (5682), 371-376 DOI: 10.1126/science.1097211
