The latest example is by parasitologist Peter Hotez, who writes in the New York Times:
There are many theories for Zika’s rapid rise, but the most plausible is that the virus mutated from an African to a pandemic strain a decade or more ago and then spread east across the Pacific from Micronesia and French Polynesia, until it struck Brazil.
After its discovery in 1947 in Uganda, Zika virus caused few human infections until the 2007 outbreak on Yap Island. The virus responsible for this and subsequent outbreaks in Pacific Islands is distinct from the African genotype, but there is no experimental evidence to suggest that sequence differences in the Asian genotype were responsible for the spread of the virus. For this reason I disagree with Dr. Hotez’ conclusion that mutation of the virus is the ‘most plausible’ explanation for its global spread. It is just as likely that the virus was in the right place at the right time to spark an outbreak in the Pacific.
We will never have experimental evidence that emergence of the Asian genotype allowed pandemic spread of Zika virus, because we cannot test the effect of individual mutations on spread of the virus in humans. Consider this experiment: infect a room of humans (and mosquitoes) with either the African or Asian genotype of Zika virus, then measure virus replication and transmission. If there is a difference between the two viruses, engineer specific mutations into the virus, reinfect another batch of humans, and continue until the responsible mutations are identified. Obviously we cannot do such an experiment! We could instead use animal models, but these have limitations in extrapolating results to humans. For this reason we have never identified any specific mutation that allows an animal virus to replicate more efficiently in humans.
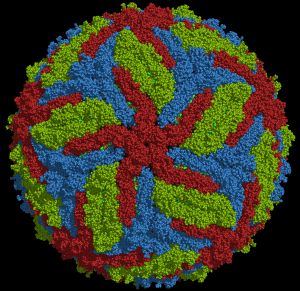
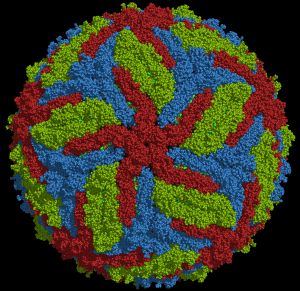
The same experimental limitations do not apply to animals. An example is Chikungunya virus, spread by Aedes ageyptii mosquitoes. Before 2004, outbreaks of infection were largely confined to developing countries in Africa and Asia. The virus subsequently spread globally, due to a single amino acid change in the envelope glycoprotein which allows efficient replication in Aedes albopictus, a mosquito with a greater range than A. ageyptii. It was possible to prove this point by assessing the effects of changing this single amino acid on virus replication in mosquitoes. The same experiment cannot be done in humans.
There is no evidence that the Asian genotype of Zika virus is any more competent to replicate in mosquitoes than the African strain. Results of a study of replication of Asian genotypes of Zika virus revealed that Aedes aegypti and Aedes albopictus are not very good vectors for transmitting ZIKV. The authors smartly suggest that “other factors such as the large naïve population for ZIKV and the high densities of human-biting mosquitoes contribute to the rapid spread of ZIKV during the current outbreak.” In other words, don’t blame the Zika virus genome for the expanded range of the virus.
The Zika virus that has been spreading in Brazil, and which has been associated with microcephaly, shares a common ancestor with the Asian genotype. In a recent study of the genomes of 7 Brazilian isolates, there was no evidence that specific mutations are associated with microcephaly. Those authors conclude (also smartly):
Factors other than viral genetic differences may be important for the proposed pathogenesis of ZIKV; hypothesized factors include co-infection with Chikungunya virus, previous infection with Dengue virus, or differences in human genetic predisposition to disease.
It’s easy to blame mutations in the viral genome for novel patterns of transmission or pathogenesis. Viral mutations arise during every replication cycle, due to errors made by viral enzymes as they copy nucleic acids. RNA viruses are the masters of mutation, because, unlike the polymerases of DNA viruses, RNA polymerases cannot correct any errors that arise. As viruses spread globally through different human populations, it is not surprising that different genotypes are selected. These may reflect adaptation to various selective pressures, including different humans, vectors, climate, or geography. There is no reason to assume that such changes influence virulence, disease patterns, or transmission in humans. Whether they do so can never be tested in humans.
Blaming the viral genome is nothing new. At the onset of the 2014 Ebolavirus outbreak in West Africa there were many claims that the unprecedented size of the outbreak was a consequence of mutations in the viral genome. Genomic analysis of isolates early in the epidemic suggested that the large number of infections was leading to rates of mutation not previously observed. This work lead to dubious claims of “Ebolavirus mutating rapidly as it spreads” and Ebolavirus is mutating (Time Magazine). Richard Preston, in the New Yorker article Ebola Wars quoted scientist Lisa Hensley:
In the lab in Liberia, Lisa Hensley and her colleagues had noticed something eerie in some of the blood samples they were testing. In those samples, Ebola particles were growing to a concentration much greater than had been seen in samples of human blood from previous outbreaks. Some blood samples seemed to be supercharged with Ebola. This, too, would benefit the virus, by enhancing its odds of reaching the next victim. Is it getting better at replicating as it goes from person to person? Hensley said.
And let’s not forget the absurd speculation, fueled by these data, that Ebolavirus would go airborne.
Within a year all this nonsense was proven wrong. Ebolavirus had not sustained mutations any faster than in previous outbreaks. Furthermore, the observed mtuations did not change the virus into a more dangerous strain.
Go back to any viral outbreak – MERS-coronavirus, SARS-coronavirus, influenza virus, HIV-1 – and you will find the same story line. Mutation of the virus is leading to more virulence, transmission, spread. But in no case has cause and effect been proven.
Let’s stop blaming viral mutation rates for altered patterns of virus spread and pathogenesis. More likely determinants include susceptibility of human populations, immune status, vector availability, and globalization, to name just a few. Not as spectacular as ‘THE VIRUS IS MUTATING!’, but nearer to the truth.

Comments are closed.