A property of N. meningitidis that makes it cause disease is resistance to complement, a collection of proteins in the blood that help clear pathogens. N. meningitidis has evolved several mechanisms to avoid destruction by complement, including the production of a polysaccharide capsule, addition of sialic acid to a component of the bacterial outer membrane, and the production of a protein that binds one of the complement proteins. It is not clear why a commensal organism would have evolved such evasion mechansims – invading the blood and the brain are dead ends, as they do not lead to transmission to a new host.
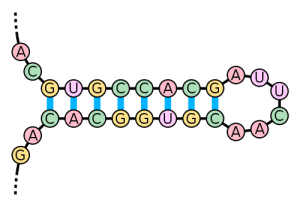
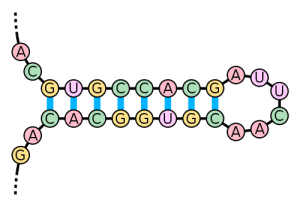
An answer to this question comes from the finding that N. meningitidis proteins essential for resistance to complement are under the control of an RNA thermosensor. This control element is an RNA stem loop structure (pictured) formed by base pairing of local sequences within the RNA. Buried in the base-paired stem is a short sequence called the ribosome binding site that is essential for translation of the mRNAs into protein. At 30°C, the stem loop structure is intact, preventing binding of ribosomes to the mRNA; protein synthesis is blocked. At elevated temperatures – 37 or 40°C – abundant protein synthesis takes place, because the RNA secondary structure is denatured, allowing ribosomes to more efficiently access the ribosome binding site on the mRNA.
How do these findings explain why N. meningitidis becomes a pathogen? The temperature of the upper respiratory tract, where the bacterium normally colonizes, is low, so the RNA sensor is intact, preventing production of proteins needed for resistance to complement. If the respiratory tract is infected with a virus, a local immune response occurs which is accompanied by high temperatures – a fever. The RNA thermosensors of N. meningitidis have evolved to sense elevated temperature and turn on the synthesis of proteins that help it to avoid destruction by the immune response. Unfortunately, inflammation also damages the mucosal barriers that normally prevent microbes from invading the underlying tissues, where they have access to the bloodstream. N. meningitidis enters the blood stream, and because it is resistant to complement, it is not cleared. The result may be septicemia and infection of the brain. Moving away from its niche in the respiratory tract is probably not part of the microbe’s plan, but rather a consequence of the fact that it has evolved to survive immune responses to other pathogens in the respiratory tract.
There is some epidemiological support for this scenario: peaks of Neisseria meningitidis disease may follow outbreaks of influenza.
The conversion of commensal bacteria into pathogens by a second infection may be more common than we know. Streptococcus pneumoniae is a human nasopharyngeal commensal that colonizes 10 to 40% of healthy individuals. The bacterium is also a leading cause of respiratory disease. There is evidence that infection with influenza virus releases S. pneumoniae bacteria from biofilms; the free-living bacteria are then able to cause respiratory disease. One of the influenza virus-induced host signals responsible for changing S. pneumoniae from a commensal to a pathogen is fever. For more on this story, listen to This Week in Microbiology #62.

I have been wondering whether we can elimate this RNA thermosensor via RNA interference technology.
great idea
last time (from 2014 no praesent) we have a hury rise of Neisseriosis events as concurrent infection in Ukrainian piggery 🙁