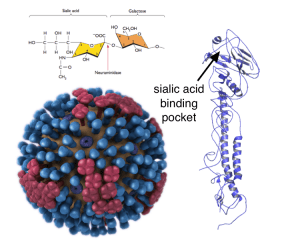
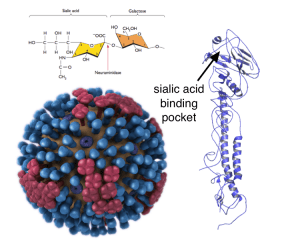
Influenza virus initiates infection by attaching to the cell surface, a process mediated by binding of the viral hemagglutinin protein (HA) to sialic acid. This sugar is found on glycoproteins, which are polypeptide chains decorated with chains of sugars. The way that sialic acid is linked to the next sugar molecule determines what kind of influenza viruses will bind. Human influenza viruses prefer to attach to sialic acids linked to the second sugar molecule via alpha-2,6 linkages, while avian influenza viruses prefer to bind to alpha-2,3 linked sialic acids. (In the image, influenza HA is shown in blue on the virion (left) and as a single polypeptide at right. Alpha-2,3 linked sialic acid is shown at top).
Adaptation of avian influenza viruses to efficiently infect humans requires that the viral HA quantitatively switches to human receptor binding – defined as high relative binding affinity to human versus avian receptors. Such a switch is caused by amino acid changes in the receptor binding site of the HA protein. The HA of the H1N1, H2N2, and H3N2 pandemic viruses are all derived from avian influenza viruses that underwent such a quantitative switch in binding from avian to human sialic acid receptors.
Avian H5N1 influenza viruses have not undergone a quantitative switch to human receptor binding, which is one of the reasons why these viruses do not undergo sustained human-to-human transmission. It has been possible to introduce specific amino acid changes in the H5 HA protein that enable these viruses to recognize human sialic acid receptors. Such changes were required to select variants of influenza H5N1 virus that transmit via aerosol among ferrets. However none of these viruses have quantitatively switched to human receptor specificity.
In the H5N1 paper, the authors compared the structure of an H5 HA bound to alpha-2,3 linked sialic acid with the structure of an H2 HA (its closest phylogenetic neighbor) bound to alpha-2,6 linked sialic acid, revealing substantial differences in the receptor binding site. To predict what residues could be changed in the H5 HA to overcome these differences, the authors developed a metric to identify amino acids within the receptor binding site that either contact the receptor or might influence the interaction. They examined these amino acids in different H5 HAs, and identified residues which might change the H5 HA to human receptor specificity. As a starting point they picked two H5 viruses that have already undergone amino acid changes believed to be important for human receptor binding. The changes were introduced into the HA of a currently circulating H5 HA by mutagenesis and then binding of the HAs to purified sialic acids and human tracheal and alveolar tissues was determined.
The HA receptor binding site amino acid changes required for aerosol transmission of H5N1 viruses in ferrets did not quantitatively switch receptor binding of a currently circulating H5 HA from avian to human (the ferret studies were done using H5N1 viruses that circulated in 2004/05). The authors note that “These residues alone cannot be used as reference points to analyze the switch in receptor specificity of currently circulating and evolving H5N1 strains”.
However introducing other amino acid changes which the authors predicted would be important did switch the H5 HA completely to human receptor binding. Only one or two amino acids changes are required for this switch in recently circulating H5 HAs.
This work is important because it defines structural features in the receptor binding site of H5 HA that are critical for quantitative switching from avian to human receptor binding, a necessary step in the acquisition of human to human transmissibility. These specific residues can be monitored in circulating H5N1 strains as indicators of a quantitative switch to human receptor specificity.
Remember that switching of H5 HA to human receptor specificity is not sufficient to gain human to human transmissibility; what other changes are needed, in which genes and how many, is anyone’s guess.
These authors have also published (in the same issue of Cell) a similar analysis of the recent avian influenza H7N9 virus which has emerged in China to infect humans for the first time. They model the binding of sialic acid in the H7 HA receptor binding site, and predict that the HA would have lower binding to human receptors compared with human-adapted H3 HAs (its closest phylogenetic neighbor). This prediction was validated by studies of the binding of the H7N9 virus to sections of human trachea: they find that staining of these tissues is less intense and extensive than of viruses with human-adapted HAs. They predict and demonstrate that a single amino acid change in the H7 HA (G228S) increases binding to human sialic acid receptors. This virus stains tracheal sections better than the H7 parental virus.
These results mean that the H7N9 virus circulating in China might be one amino acid change away from acquiring higher binding to human alpha-2,6 sialic acid receptors. I wonder why a virus with this mutation has not yet been isolated. Perhaps the one amino acid change in the viral HA exerts a fitness cost that prevents it from infecting birds or humans. Of course, as discussed above, a switch in receptor specificity is likely not sufficient for human to human transmission; changes in other genes are certainly needed. In other words, the failure of influenza H7N9 virus to transmit among humans can be partly, but not completely, explained by its binding properties to human receptors.

now we have increased structural knowledge in how to create a pandemic strain from
either old or new H5N1s : how to best choose from any of the multiple variants.
It is anticipated what the next experiments will be and that they may “succeed” soon.
But otoh, watching for these mutations in natural H5N1 is limited to
current strains which become more and more chicken-specific,
while we had no documented pandemics yet that envolved
from chicken-viruses, only swine and ducks.So that’s another limitation.
And suppose we watch these mutations in nature, what will that help us ?
We could intensify our pandemic preparedness, but we could not do much
to prevent it.
Pingback: A single amino acid change switches avian influenza H5N1 and H7N9 viruses to human receptors | Viral Bioinformatics Resource Center
Pingback: A single amino acid change switches avian influenza H5N1 and H7N9 viruses to human receptors | Ishtarmuz's Blog
Prevention would definitely not be impossible. The first thing that comes to mind is vaccination with particular, human-transmissible forms of HA. And, when you have the information of where the particular virulent strain might emerge, you can more effectively try to contain it using the more classical methods of quarantine, etc. That is, if observing them in nature will give us timely enough information.
Thank you, it was very interesting reading
A few questions though:
” Perhaps the one amino acid change in the viral HA exerts a fitness cost that prevents it from infecting birds or humans”
– Why should one amino acid change in a receptor incur a fitness cost? It seems quite unlikely, unless the sequence coding for it is a target for a particular host defense mechanism.
“Remember that switching of H5 HA to human receptor specificity is not sufficient to gain human to human transmissibility; what other changes are needed, in which genes and how many, is anyone’s guess.”
– If we are not certain which or if other changes are necessary, why couldn’t the specificity switching of H5 to alpha 2-6 sialic acid would be enough to cause human-to-human transmission? And what do you recon, which other genes would need to change for that?
that vaccination/containment didn’t work in the past.and experts don’t expect it to stop a pandemic,
except maybe in very special situations with early detections in rural areas.
But not Mexico City or Shanghai.A potential pandemic creator could choose the
initial location(s) and timing accordingly.
Your argument is somewhat valid, but what it is essentially about, is the ever-present possibility that someone misuses the products of scientific research. While this is always a possibility, it is not strong enough to warrant the discontinuation of research into “sensitive areas”. Although, in this case, it does deserve a second thought as to how the information should have been publicized.
So let us see the possibilities:
1) If we are aware that antigenic shift (or in this case, antigenic drift) may occur soon, with potentially catastrophic consequences, it is obvious that we must know more about this. I.e. research is necessary.
2) Once you have learned something about it, how do you go about publicizing it? If you only release it to closed communities, e.g. WHO, etc, then you limit the number of people who are exposed to the problem, and can potentially find a solution. You also limit the resources available for dealing with this problem.Also, one would get no credit for work that is not officially publicized, so if this research is done in a university, then the researcher will risk his funding, and also loses any opportunity for public recognition, if the work goes unpublicized. But, then again, releasing it for everyone to read, is a major security issue. Even despite the fact that in order to induce these mutations for malicious purposes, one would need very sophisticated laboratory and equipment.
Perhaps there could be a solution found in creating restricted access networks, which could only be accessed by accredited, relevant researchers, but would not be institutionalized, as most organizations containing classified information are.
Also,
“that vaccination/containment didn’t work in the past.and experts don’t expect it to stop a pandemic…”
– could you provide some specific references?
Michael wrote:
> Your argument is somewhat valid, but what it is essentially about, is the ever-present
> possibility that someone misuses the products of scientific research.
I think it’s particularly important in this case. “Half of mankind could die” as one of the world’s
leading flu-researchers said.
> While this is always a possibility, it is not strong enough to warrant the discontinuation
> of research into “sensitive areas”. Although, in this case, it does deserve a second thought
> as to how the information should have been publicized.
how was it publicized when they invented the atombomb ?
> So let us see the possibilities:
> 1) If we are aware that antigenic shift (or in this case, antigenic drift) may occur soon,
> with potentially catastrophic consequences, it is obvious that we must know more
> about this. I.e. research is necessary.
> 2) Once you have learned something about it, how do you go about publicizing it?
selected trusted researchers. As NSABB had first suggested until they recognized
the US-legal system is not suitable for that and FOI-requests would succeed.
(change the laws !)
> If you only release it to closed communities, e.g. WHO, etc, then you limit the number
> of people who are exposed to the problem, and can potentially find a solution.
yes. Nothing new. We also do that by biosafety requirements, grants etc.
> You also limit the resources available for dealing with this problem.Also, one would get
> no credit for work that is not officially publicized, so if this research is done in a university,
> then the researcher will risk his funding, and also loses any opportunity for public recognition,
> if the work goes unpublicized.
oh dear. Just give them money,rewards,titles,jobs as usual, as they earn it.
It’s the governments that decide this.
> But, then again, releasing it for everyone to read, is a major security issue. Even despite
> the fact that in order to induce these mutations for malicious purposes, one would need
> very sophisticated laboratory and equipment.
yes, but it’s rapidly becoming cheaper and easier and more common.
We must think in advance.
> Perhaps there could be a solution found in creating restricted access networks,
> which could only be accessed by accredited, relevant researchers, but would not
> be institutionalized, as most organizations containing classified information are.
good.
> Also,
> “that vaccination/containment didn’t work in the past.and experts don’t expect
> it to stop a pandemic…”
> – could you provide some specific references?
I remember Bush’s famous attempt in 2005:
http://effectmeasure.blogspot.de/2005/10/annas-on-bush-quarantine.html
then I remember the survey from UK, 2007:
http://www.flutrackers.com/forum/attachment.php?attachmentid=16528
there were lots of papers, i.e. in 2006,2007 (Longini,Ferguson,)
see also all the national pandemic plans
keywords: modelling,pandemic,”NPI”s non-pharmaceutical interventions
(I remember one in late 2006 that was more optimistic , using many vaccines
antivirals, strict measures – (link) but probably won’t work in 3rd world
and just one wave
Once the mechanism is understood, I see the potential for dozends, hundreds
of pandemi9c strains. And that’s just flu.
We need international agreement on this, instead we are getting a race
who will be the first to create a pandemic capable virus.
And many of these efforts are presumably nonpublic because of fear
of ethics discussion. E.g. Fouchier announced that he is not seeking
for more passaging, but only after the discussion started.
Secretly they and others are probably still trying this or will do.
Then, if they succeed, yes, what then ? Publish or wait until
someone else finds it ?
Pingback: Bookmarks for June 13th from 16:46 to 18:33
Pingback: Horses Prefer Bio-Hoof (5 Lb Powder) - Muscle Building
This H7N9 and H5N1 is being studied in ducks and poultry though. What if it mutates ans infects another species other than swine such as deer or fish. would this change the possibilities? Fish and deer are often obtained from the wild for consumption and what if anything is being done to investigate the mass animal deaths experienced globally. They all are dying of reporatory failure and local conservation dept label it as “unknown” I like my DEC guys but they are not biologists.